A Message from the Chairman
One of the great delights of being Chairman of WMAS is the opportunities to spend time with staff hearing about their work and seeing the difference they make to patients.
While it is often quoted that staff are the most important part of any organisation, I can say that this is 100% true of our Trust. Whichever part of the Trust they work in, they all contribute in their own way to supporting patient care.
As someone who started their career in the NHS as a scientist, research and development has always been hugely important to me. The Trust enrolled around 1,000 participants into more than a dozen different research studies last year, all with the aim of improving patient care and staff wellbeing and this is something I am especially proud of.
Innovation is a cornerstone of our Trust and one innovation that was introduced this year did grab my attention. Our Education and Training team have been working with a software company to develop a state-of-the-art virtual reality driving simulator to supplement on the road ‘blue light’ training with more complex and challenging scenarios that would not occur under everyday driving conditions. We have already had interest from other emergency services who are keen to see how they might follow suit within their blue light driver training with the Trust.
Another area that I am passionate about is patient safety. Over the last year, the Trust introduced the Patient Safety Incident Response (PSIR), a new way of looking at how we review incidents that happen and, more importantly, what we can do to stop them happening again. The feedback that we have had from both staff and external bodies has been very positive and that can only be a sign of the success of the implementation and the hard work of the team.
Continuing the work begun last year in developing ways to support our staff, this year we appointed a ‘People Promise’ Manager to support colleagues.
While we are rightly proud of the work that we do to recruit new staff, we are working equally hard to retain staff. We have seen the number of staff leaving slow considerably and have the lowest turnover of staff in the ambulance sector, which suggests that we are making good progress.
As you will read in the Chief Executive’s Review of the year, hospital handover delays remain a very real issue for us and the Board took the difficult decision to raise the risk rating to the maximum level, to register our concern that patients are coming to harm due to the delays.
The Board are rightly concerned about the impact on patients but also on staff who are routinely subjected to missed meal breaks and late finishes that impact family time. I know I speak for the whole Board when I say it is our biggest concern and one that we will do all we can to find solutions to.
Board membership has changed a little this year. We welcomed as new non-executive directors, nurse Suzanne Banks and Sukhjeeven Nat, who comes from a finance background. They replace Wendy Farrington-Chadd and Narinder Kaur Kooner whose terms had ended.
From an Executive position, we were sad to see our Medical Director, Dr Alison Walker, step down at the end of November. While leaving us in a formal role, Alison will continue to be part of our Trust through her national work.
We were delighted to welcome Dr Richard Steyn as Alison’s replacement. Richard has worked with the Trust for decades in his role as an emergency doctor. His reputation in the NHS is unparallelled and we are delighted that he has joined us in a more formal role.
Finally, on behalf of the Board, I want to thank all staff, wherever they work in the organisation, for all that they have done during this last year. Equally, my thanks to the many students and volunteers who also work with us.
Together, your dedication to saving lives and helping people in their hour of need is second to none and I thank every one of you for what you have done over the last 12 months.
Prof. Ian Cumming OBE , Chair, West Midlands Ambulance Service University NHS Foundation Trust
Chief Executive’s Review 2024-25
Last year I said that I was trying to find a different way to start my annual review, but sadly, it is the same old problems that largely marked out the year: hospital handover delays and a tough financial climate.
We lost a staggering 380,000 hours of crew time as ambulances waited to offload their patients outside A&E. That’s equivalent to taking 86 ambulances off the road and putting them in a car park every day!
We have once again taken difficult decisions to prioritise frontline operations, bring in a balanced budget and work with our staff to improve our response time performance compared to last year.
We will be one of only a few services to achieve the target of getting to the stretch target of reaching Category 2 calls in under 30 minutes.
While this is good news it must be remembered that the full target is 18 minutes, so we still have some considerable distance to go and the only way we will be able to reach that target is through a reduction in hospital handover delays.
In more positive news, we continue to have the best call taking in the country with the fewest number of calls waiting over two minutes to be answered, despite receiving 1.78 million emergency 999 calls last year.
Another area where we lead the country is our ability to deal with cases in our control rooms. Over 20% are now dealt with by our experienced team of paramedics and nurses. In addition, we refer over 400 calls a day to urgent care providers which allows patients to get the care that best meets their needs.
We have seen real progress in the way that we deal with mental health patients. We have seen a significant rise in such cases since the COVID-19 pandemic and as a result we have invested in specialist vehicles and staff to tackle this hugely important issue. Figures from the Home Office shows that we are the leading ambulance Trust in England and Wales when it comes to the patients detained under section 136 of the Mental Health Act.
Our Patient Transport Services have once again had an excellent year despite incredibly challenging times. We have significantly improved our performance despite rising numbers of cases. The feedback we receive shows just how much the efforts of staff means to their patients.
It has been a busy year for our Community First Responders, who dealt with around 1,000 cases a month, we have, therefore, increased the number of Community First Responders we have assisting us.
The latest data from NHS England shows that we continue to be the most efficient Ambulance Trust in the country, with a bigger percentage of staff working in frontline roles. As well as taking on more staff, fewer of our existing staff are choosing to leave us. We have the lowest turnover in the ambulance sector and one of the lowest in the NHS.
While far too many patients have waited much longer than we would want to get the help they need, I have been moved by the record number of patients who have taken the time to contact us to say, ‘thank you’. While none of our staff do the job for that reason, there is no question it makes a huge difference to the staff who helped you. It is truly appreciated.
I was pleased to see a rise in the number of staff using the Freedom to Speak Up (FTSU) service during the year. While this might seem an odd statement to make, it means that colleagues have the confidence to raise issues which allows us to make improvements. Of course, this is only one of many different ways that staff can do so. The work of our Guardians and the team of staff ambassadors who work on each of our sites is having a real impact on the belief amongst staff that they can and should raise concerns which can only be a good thing.
Sadly, staff continue to be on the receiving end of violence and aggression on an all too regular basis. It is one of the reasons why we support the Association of Ambulance Chief Executives (AACE) #WorkWithoutFear campaign.
We have seen an almost 100% increase in violence in recent years. This is not just physical violence to staff on the road; our call assessors have been threatened in the most horrendous ways.
While I often concentrate on the work of our frontline staff, I would also like to take a moment to pay tribute to the outstanding work of our support services. Be that the team who maintain and clean our ambulances, the stores team who move literally millions of items every year or those who work in our corporate teams.
May I finish by saying how enormously proud I am of each of our staff, students and volunteers; governors and non-executive directors, please accept my enormous thanks and pass on my personal thanks to your family members that have loved and supported you to enable you to give your best every day, saving lives across the West Midlands. I firmly believe that the public of the West Midlands should be justifiably proud of the team that protects them.
Thank you for all that you do.
Anthony C. Marsh, Chief Executive Officer
Performance Report
Overview of performance
Chief Executive’s summary of Trust performance
The Annual Report is a chance for us to look back over the last 12 months and look at what went well and what could be improved. As with most years it was one of highs and lows; while we saw a serious deterioration in the level of hospital handover delays, the actions we took mean that we have been able to get to more patients more quickly than we did the previous year.
After 2023 to 2024 there was real hope that hospital handover delays would continue to improve. Sadly, that proved to be a short-lived hope. April through to July saw a significant deterioration in the situation compared to the previous year. While the summer months brought a brief respite, since October we have seen the worst delays on record each month with December bringing the biggest ever loss at 53,231 hours. That is equivalent to losing 140 ambulances off the road! Instead of an improvement, we have seen an increase from 255,000 hours grown to 380,000 hours this year, an almost 50% worsening of the situation.
Despite this, we have continued the good work of last year and our Category 2 Mean has dropped from 36 minutes and 3 seconds to 29 minutes and 5 seconds. Equally, our 999 call handling has remained the best in the country with the lowest number of over two-minute calls. Whilst this is progress, the Category 2 performance is still well above the national target of 18 minutes, something we used to achieve every year. Similarly, we would not want to see any 999 call waiting over two minutes to be answered.
To put this into context, in 2019 to 2020, the year before the COVID-19 pandemic, we lost 87,646 hours of ambulance time due to handover delays. Sadly, we have continued to see incidents where harm has come to patients simply because we did not arrive quickly enough. The maximum time a patient waited to be handed over during the last 12 months was over 20 hours.
I cannot understate the impact these delays have had on both patients and staff. Our ability to get to patients quickly has been severely impacted. The reality is that we do not get to heart attack and stroke patients as quickly as we should and that will have a long-term impact on the quality of the patient’s life going forwards. It also pains me to see cases of elderly patients who have had a fall, waiting hours on the floor, sometimes outside in all kinds of weather for multiple hours. It is truly heartbreaking.
The issue was highlighted in our last Care Quality Commission inspection report: “Ambulances were queuing for hours at A&E departments due to handover delays, which impacted on people’s care and wellbeing. This resulted in longer response times, it also had a negative effect on staff, who were doing their best to provide safe care and treatment to people.”
The report resulted in the regulator taking action against the Trust which led to WMAS putting together an action plan that has led to the improvement in performance. As previously mentioned, this is good progress, but there is still a long way to go and we are still failing people who often desperately need our help due to the ongoing hospital delays.
The Trust Board took the extraordinary step in 2022 of raising the Risk Rating to 25 – the highest possible – for two areas: the level of hospital handover delays and the time it takes for us to respond, both of which result in harm coming to patients. While I am pleased that we reduced that, sadly as the delays got worse and worse we once again moved the rating back to 25 in November 2024.
There has been progress, and we are pleased that the Planning Guidance from NHS England for 2025 to 2026 contains reference to no ambulance waiting over 45 minutes to offload and a clear direction of travel to get that back to the national target of no patient waiting longer that 15 minutes for a clinical handover. Recent figures from NHS England show the tens of millions of pounds that could be saved if that were to happen, never mind the lives that would not be impacted negatively.
Despite what is a very concerning picture, there are some positives. The fact that there are some is down to the outstanding work of our staff and volunteers, right across this Trust, who do an amazing job in trying to provide the best care possible for our patients.
We continue to have the best call answering performance in the country. The data from BT shows that we have the smallest number of occasions when it has taken more than two minutes to answer a 999 call. Last year we had 202, down from 1,200 the previous year. Nationally there were 91,824 such cases. What is remarkable is that so few calls waited over two minutes when the teams in our control rooms in Stafford and Brierley Hill took 1,576,636 calls during the year.
At a time when we need to work harder than ever to meet the challenges we face, data shows that the average number of patients an ambulance crew see during a shift remains far lower than in the past. At one point, crews were seeing on average almost eight patients per 12 hour shift. The total in 2024 to 2025 was four, which is slightly up on the previous year. Sadly though, we also know that some crews end up seeing only one patient because they have taken their first patient to hospital and have then not moved due to the delays handing over.
The Trust continues to do all it can to assist the wider health economy by finding new and innovative ways to treat patients without the need to convey them to an emergency department. We now take only slightly above 40% of patients to an emergency department. The work of our Clinical Validation Team is leading the way in the country. Every day, over 400 patients will be referred to urgent care services in other parts of the NHS so that patients can get the most appropriate treatment for their condition. The work of the experienced paramedics and nurses, means that over 20% of patients are dealt with over the phone; the best in the country and on some days that has been well over 25%. Their work is supported by having a paramedic on every ambulance; this allows us to treat many more patients at the scene of the incident.
The ‘Call Before you Convey’ scheme, which allows crews to speak to another clinician, has helped thousands of additional patients to be diverted from Accident and Emergency departments. We continue to monitor the clinical data to see if there are any patterns that mean we can do more to refine the process so that each patient gets what is best for them.
It is hard to imagine just how difficult and frustrating the last few years have been for staff. We have been able to triangulate the impact on them through the results in our staff survey, the answers we get from colleagues and through the work of our Health and Wellbeing team, Staff Advice and Liaison Service and the conversations our managers have with staff. We absolutely recognise the impact these delays have on the health and wellbeing of our staff as they do all they can to cope with these very difficult conditions. It is why we have invested heavily in ensuring there is 24-hour support for staff on all of our hubs as well as improvements in the wellbeing support available such as employing three mental wellbeing practitioners as well as dedicated peer to peer and online support.
While the staff on the frontline, those in our control rooms and the hundreds who provide non-emergency services are the face that most people know us for, there is also a small army of people who support them. These are the people who enable those staff to carry out their vital roles. I am thinking of our mechanics, those that prepare our ambulances and our education and training department, but also the key corporate functions who make sure the organisation works effectively, safely and efficiently such as those in finance, IT, workforce, organisational development, recruitment, supplies and distribution, and press and communications etc. They may not be as high profile, but they play a vital role nonetheless.
The finances of the NHS often hit the national headlines, and this year has been no different. We face one of the toughest financial climates I have ever seen in my 40 years in the NHS. This results in difficult decisions, but as an organisation we are committed to ensuring we utilise our resources effectively and will continue to invest the maximum amount in our frontline services. The latest data from NHS England shows that we are the most efficient ambulance service in the country. We will face each challenge head on and make the necessary changes to provide the highest standard of clinical care to our patients. With these commitments we will continue to strive to perform at the highest levels possible whilst also achieve the requirement to break even, thereby meeting all of our required financial duties.
If I can conclude by thanking the staff and students within this Trust and also the volunteers who support us. Not only the community first responders who give up their time to support their local communities but also those that support organisations such as the two air ambulance charities and emergency doctors who respond to some of our most seriously ill and injured patients. Their work cannot be underestimated. Thanks also to our governors and non-executive directors who also do so much to support the work of the Trust.
Over and over again, the dedication and commitment of our staff, students and volunteers shines through and makes us the organisation we are. Please accept my grateful thanks for all that you do. There is no question that your work, whichever part of the organisation you are in, helps to save lives and that is something we should all be immensely proud of. Thank you to you all.
Anthony C. Marsh, Chief Executive Officer
A brief history of the Trust
The former West Midlands Ambulance Service NHS Trust was created on 1 July 2006 with the amalgamation of the original West Midlands Ambulance Service NHS Trust, Coventry and Warwickshire Ambulance NHS Trust and Hereford and Worcester Ambulance Service NHS Trust. Staffordshire Ambulance Service NHS Trust joined in October 2007.
West Midlands Ambulance Service became an NHS Foundation Trust in 2013.
On 1st November 2018, we became the first University Ambulance Service in the country after a Memorandum of Understanding was signed with the University of Wolverhampton
Following a public consultation, the name of the Trust was changed to West Midlands Ambulance Service University NHS Foundation Trust.
Trust activities, business model and environment
Urgent and Emergency Services (999)
This is the best known part of the Trust and deals with the emergency and urgent calls. And is directed from the three Integrated Emergency and Urgent Care Centres (IEUCs) two of which are at Brierley Hill near Dudley, and the third located in Stafford which answer and assess 999 calls.
Call taking and assessment
The Trust provides 24/7 emergency response services comprising 999 call handling, and response.
When a 999 call is made the caller is put through to a BT operator who asks what service they need – If it’s an ambulance, they will be put through automatically to their location to their local ambulance service, based on their own location.
Our emergency call centres manage over 4,300 calls each day.
When your call is transferred, you will speak to one of our call assessors who will ask you a number of questions to help us give you important first aid advice while our staff establish the most appropriate response.
Clinical Validation
Not all calls require an ambulance response; some 999 calls are dealt with by our Clinical Validation Team (CVT) within in our Emergency Operations Centre. This team comprises paramedics and nurses specially trained to help patients who have called 999 needing medical help.
Ambulance Response
The Trust dispatches ambulances from fifteen Hubs located across the West Midlands
Other Services
Non-Emergency Patient Transport Service
The Trust operates Non-Emergency Patient Transport Service contracts across Birmingham, the Black Country, Coventry and Warwickshire and Cheshire.
There are 12 operational Non-Emergency Patient Transport Service bases, including staff that are home-based and 4 control rooms. The Non-Emergency Patient Transport Service transports just under 1 million patient journeys per annum. They transfer and transport eligible patients to and from hospital appointments, transfer between hospital sites, deal with routine admissions, discharges and for continuing treatments such as renal dialysis and oncology. The Non-Emergency Patient Transport Service also provides a high-dependency tier across Birmingham, the Black Country and Coventry and Warwickshire.
Emergency Preparedness, Resilience and Response (EPRR)
EPPR is a small but vitally important part of the organisation, responsible for planning and responding to significant and major incidents within the region, as well as providing medical support for large gatherings such as football matches and festivals.
Other Commercial Services
The Healthcare Logistics service provides a wide range of services for mainly NHS customers in Staffordshire and Stoke-on-Trent including clinical waste and mail collection, medical forms and supplies deliveries and specimen collections.
The Trust’s Commercial Call Centre offers message handling for NHS, public sector and private sector clients, including GP in hours call answering, UK Health Security Agency, National Burns Bed Bureau.
The Trust’s Operating Environment
Geographical coverage
Services are provided over 5,000 square miles of Herefordshire, Worcestershire, Shropshire, Coventry, Warwickshire, Staffordshire, Birmingham, Solihull, and the Black Country.
Population served
The Trust serves 6 million people across the West Midlands.
Diversity of population
The West Midlands includes the second largest urban area in the country, covering Birmingham, Solihull and the Black Country where 43% of the population live.
Birmingham is England’s second largest city and the main population centre in the West Midlands, second only to the capital in terms of its ethnic diversity, which makes it vital that we work closely with the many different communities we serve, listening and responding to their suggestions and comments to ensure that our service meets the needs of everyone in the region.
The region is also well known for some of the most remote and beautiful countryside in the country including the Staffordshire Moorlands and the Welsh Marches on the borders of Herefordshire and Shropshire with Wales.
Trust Structure and Resources
Staffing
The Trust employs over 7,200 staff of which 4,439 are frontline paramedics and technicians and 902 provide non-emergency patient transport services.
Volunteers
The Trust is supported by a volunteer network of over 450 Community First Responders (CFRs) providing early intervention in life critical emergency situations and training in their communities on the use of defibrillators and resuscitation techniques. This reached over 24,000 members of the public last year.
Facilities
Ambulance responses are provided from 15 operational ambulance bases across the region. 999 call handling and call-based responses are provided from two emergency operations centres.
Fleet Assets
The Trust operates over 1,000 vehicles including emergency ambulances, non-emergency patient transport service vehicles and specialist resources such as major incident vehicles.
Vision, Values and Objectives
Vision
Delivering the right patient care, in the right place, at the right time, through a skilled and committed workforce, in partnership with local health economies.
Our vision places the patient at the centre of everything we do and provides a focus through which we deliver safe, high quality patient care and treatment, underpinned by sound values and a commitment to collaborative working with staff, members, volunteers and stakeholders.
Values
Excellence
A high performing organisation with professional, engaged, empowered and valued staff who learn from each other to be the best we can together in order to deliver the best possible care and outcomes for our patients and service users. Cutting edge and innovative using the best evidence.
Integrity
We all do the right thing for our staff, volunteers and students, our patients and service users, the organisation and the system with candour.
Compassion
We believe that showing genuine concern about the needs of others through our actions fosters appreciation and tolerance, leading to a sense of safety in the workplace.
Inclusivity
We treat everyone with dignity, respect, fairness and integrity, valuing difference.
Accountability
We are committed to upholding our values and behaviours and holding others to account for them.
Strategic Objectives
Strategic Objective 1: Safety, Quality and Excellence. Our Commitment to provide the best care for all patients.
Strategic Objective 2: A great place to work for all. Creating the best environment for staff to flourish.
Strategic Objective 3: Effective planning and use of resources. Continued efficiency of operation and financial control.
Strategic Objective 4: Innovation and Transformation. Developing the best technology and services to support patient care.
Strategic Objective 5: Collaboration and Engagement. Working in partnership to deliver seamless patient care.
The delivery of these objectives is monitored through the implementation plans of a suite of enabling strategies including:
- Clinical Strategy
- Quality Strategy
- Communications and Engagement Strategy
- Risk Management Strategy
- Security Strategy
- Sustainability Strategy
- Freedom To Speak Up Strategy
- Equality, Diversity and Inclusion Strategy
- IT, Data and Digital Strategy
- Commercial Services Strategy
- Fleet Strategy
- Estates Strategy
- Operations Strategy
- Finance Strategy
- People Strategy
- Volunteering Strategy
These strategies are in the process of being streamlined into fewer, more comprehensive documents. This is taking place as the documents are due for a refresh.
Principal risks, impacts, mitigation and management
Risks
The Board Assurance Framework (BAF) is a tool to support the Board in carrying out its duties. The Board Assurance Framework brings together in one place all the relevant risk information on the threats to the achievement of the Board’s strategic objectives. The most significant risk during the year was the impact of hospital handover delays. This is discussed in detail in the Chief Executive’s Overview of Performance on page 9.
Risk SO1 – Handover Delays
Organisational Impact
- Patient harm/Risk of Patient death/ Risk of patient deterioration
- Increased waiting time/delay for patients in the community waiting for 999 response
- WMAS – Failure to adequately observe a patient, HALO unable to see full number of patients
- Staff Welfare and Morale – Staff Increased sickness/fatigue
- Emotional and mental wellbeing of patient and WMAS staff
- Skill decay of staff and lack of exposure
- Reduction in CQC Outstanding rating – hospital delays referenced as the main cause for the CQC Improvement Notice
- Exposure to violence and aggression from Patients and Patients’ relatives
- Staff in EOCs raised stress levels speaking to callers for protracted periods, or on numerous occasions
- Performance reduction
- Adverse media coverage and loss of public confidence
Risk SO1 – Handover Delays
Actions undertaken
- Ambulance Handover Delays Board report
- Gold Commander “reactive protocol” to specific cases in the event of significant Patient delays and Ambulance Turnarounds
- HALO Cohorting SOP
- Hospital desk 24/7 hours of operation.
- On Call teams, Gold and SOM’s engaged in reporting delays and supporting at sites with ++ delays
- SOC and EOC management of Hospital delays, escalation of each delay to NHSE, CCG and Hospital WMAS
- Escalation Process – HALO to OM/SOM
- Regular meetings between WMAS and Hospital
- Regular Liaison with Hospital Leads from WMAS
- Escalation Plan this is monitored by SOC during times of pressure at acute sites
- Divert processes
- Implementation and monitoring of the Conveyance Policy
- REAP and Surge Plan
- Operational Performance Plans
Risk SO2 – Calls Waiting
Organisational Impact
- Continued stacking of calls.
- Failure of category 2 performance.
- Continued patient delay and harm.
- IEUC staff fatigue and deterioration to their health and wellbeing due to increased activity and inability to allocate ambulance to waiting patients.
- Call takers also impacted because of numerous duplicate calls received, chasing estimated time of arrival for ambulance, marked increase in call volume (approx. 22% of calls received during October 2021 were duplicates against 10% in October 2020, and 12% October 2019)
- Sickness in IEUC and E&U ops has increased due to stress and anxiety one of the main causes.
- Organisational reputation risk and litigation due to delays responding to patients and public confidence in the service as seen in recent press articles.
Risk SO2 – Calls Waiting
Actions undertaken
- UCR Lead appointed to post.
- Robust IEUC Policies, Procedures and protocols.
- Engagement with partner agencies.
- Significant investment and increases in operational staffing levels.
- Significant increase in Call Assessor numbers. Current establishment circa above 420 trained call assessors.
- Resource output producing above 350 frontline ambulances at peak per day.
- Surge demand management plan (SDMP) now embedded within the EOC and utilised as required.
- Implementation of the SCC (excluding Staffordshire).
Risk management
For a full description of the Trust’s approach to risk identification and management mechanisms, see Risk and Control Framework within the Annual Governance Statement below, on page 85.
The importance of engaging all staff in risk management
Staff have an important role to play in identifying, assessing and managing risk and the Trust encourages a culture of openness. Staff are able to raise risks directly with managers, through electronic reporting, whistleblowing and freedom to speak up, team meetings, via Staff Side representatives, partnership forums, and with Executive and Non-Executive Directors during their visits to Trust premises.
Going Concern Disclosure
At the meeting of the Trust’s Audit Committee on the 18 March 2025 a detailed discussion took place on the application of the Going Concern Concept to the Trust.
Taking account of the recommendation of the Audit Committee, and after considering the current financial and operational position of the Trust, the Directors at the meeting of the Board of Directors held on 26 March 2025 approved a resolution that there are no material uncertainties that may cast significant doubt about the Trust’s ability to continue as a going concern and therefore there is a reasonable expectation that the Trust has adequate resources to continue in operational existence for the foreseeable future.
For this reason, the Board of Directors continue to adopt the Going Concern basis in preparing the accounts for 2024 to 25.
Summary of Performance
Operational performance
Performance by Integrated Care System 1 April 2024 to 31 March 2025
| Integrated Care System 1 | Category 1 Mean | Category 190TH | Category 2 Mean | Category 290TH | Category 390TH | Category 490TH |
|---|---|---|---|---|---|---|
| Birmingham and Solihull ICS | 6:55 | 11:33 | 26:17 | 61:47 | 421:21 | 544:46 |
| Black Country ICS | 6:44 | 11:08 | 21:39 | 47:58 | 326:24 | 313:11 |
| Coventry and Warwickshire ICS | 8:57 | 16:02 | 29:30 | 62:13 | 290:33 | 300:47 |
| Hereford and Worcestershire ICS | 10:42 | 20:39 | 31:59 | 67:04 | 313:32 | 354:31 |
| Shropshire, Telford and Wrekin ICS | 11:55 | 24:13 | 37:17 | 79:04 | 336:14 | 415:14 |
| Staffordshire and Stoke on Trent ICS | 8:58 | 15:43 | 35:45 | 77:32 | 373:06 | 455:40 |
| Total | 8:15 | 14:39 | 29:05 | 64:23 | 349:44 | 404:37 |
Performance Analysis
Operational Performance
Urgent and Emergency Services (999)
The Trust is measured nationally against operational standards for Emergency and Urgent as below:
Category 1 – Calls from people with life threatening illnesses or injuries
7 minutes mean response time, 15 Minutes 90th centile response time.
Category 2 – Serious condition that requires rapid assessment (Serious injury, stroke, sepsis, major burns etc)
30 minutes mean response time, 40 Minutes 90th centile response time.
Category 3 – Urgent but not life threatening (e.g. pain control, non-emergency pregnancy)
120 Minutes 90th centile response time.
Category 4 – Non urgent but require a face to face assessment
180 Minutes 90th centile response time.
Non-Emergency Patient Transport Services
The Trust currently operates Non-Emergency Patient Transport Services contracts across Birmingham, the Black Country, Coventry and Warwickshire and Cheshire. Each contract has its own set of operational performance/quality targets and thresholds for achievement. Currently there are 47 operational Key Performance Indicators (KPIs) that we are reporting on, these include a set of standard measures in relation to punctuality both on inward and outward journeys and transfers/discharges, ensuring patients arrive for appointments promptly and are also collected in a timely manner. 2024 to 2025 has seen operational challenges across Patient Transport Services with uncertainty around contracts, increase in high mobility/complexity of patient requirements, leading to limited capacity and workforce challenges. In total the Trust achieved 36 out of 47 Non-Emergency Patient Transport Services Key Performance Indicators in 2024 to 2025.
Data Quality Policy
The Trust recognises that data quality is crucial to the delivery of fast and effective service provision. Complete, accurate and timely data is important in supporting care delivery, clinical governance, management of information, clinical audit and achieving service targets. The effective use of performance information depends on data that is robust and accurate. Sufficient high-quality information must be available to allow confidence that performance is tracked and, in particular, that the quality of key data entered by all control rooms across the region is monitored to ensure compliance with national and local requirements. There are several specific reports available on the Trust’s report portal, ORBIT, which the Emergency Operations Centre and operational managers can use to improve data quality. Additionally, a suite of automated data quality reports is circulated routinely to managers to help monitor data quality. Examples of data quality checks include Routine/Referral categorisation and the triggers for clock starts.
The Trust has a formal Data Quality Policy. The Digital and Transformation Oversight Group has responsibility for reviewing and endorsing it, and both Internal and External Audit review internal controls and undertake testing of data produced.
Quality Performance
Ambulance Quality Indicators – National Audits
Ambulance Services are not included in the formal National Clinical Audit programme, however, during 2024 to 2025 the Trust participated in the following National Ambulance Clinical Quality Indicators Audits:
Care of ST Elevation Myocardial Infarction (STEMI)
This is a type of heart attack that can be diagnosed in the pre-hospital environment. Patients diagnosed with this condition are often taken directly to specialist centres that can undertake Primary Percutaneous Coronary Intervention (PPCI).
Audit Element
Percentage of patients with a pre-existing diagnosis of suspected ST elevation myocardial infarction who received an appropriate care bundle from the Trust during the reporting period.
In patients diagnosed with STEMI it is important to get them to a Primary Percutaneous Coronary Intervention (PPCI) centre as quickly as possible – MINAP records the time that the PPCI balloon is inflated by the hospital.
Audit Element
The Trust measures 999 Call to catheter insertion by the mean and 90th percentile.
Care of Patients in Cardiac Arrest
In patients who suffer an out of hospital cardiac arrest the delivery of early access, early CPR, early defibrillation and early advanced cardiac life support is vital to reduce the proportion of patients who die from out of hospital cardiac arrest. The Trust provides data to the Out of Hospital Cardiac Arrest Outcomes Registry.
Audit Element
Percentage of patients with out of hospital cardiac arrest who have return of spontaneous circulation on arrival at hospital and patients that survive to hospital discharge and a care bundle for treatment given post return of spontaneous circulation.
| Ref. | Clinical audit title | Ref. | Clinical audit title |
|---|---|---|---|
| CG002 | PGD Audit | CG098 | Non traumatic chest pain >=18 years discharged at scene |
| CG080 | Administration of Morphine Audit | CG099 | Head Injury discharged at scene discharged at scene |
| CG091 | Adrenaline Administration | CG100 | Feverish Illness in children discharged at scene |
| CG092 | Naloxone Administration | CG102 | Blood Ketone Audit |
| CG094 | Activated Charcoal | CG103 | Management of Sepsis |
| CG095 | Co-amoxiclav administration | CG104 | Management of Asthma In Children |
| CG043 | Management of Paediatric Pain | CG105 | Mental Capacity Act |
| CG061 | Maternity Management | CG106 | Management of Overdose |
| CG089 | Post-partum haemorrhage (PPH) management | CG107 | MERIT PHEA |
| CG097 | Falls >=65 discharged at scene | CG108 | MERIT Transfusion |
Ambulance Quality Indicators
- Care of ST Elevation Myocardial Infarction (STEMI) Percentage of patients with a pre-existing diagnosis of suspected ST elevation myocardial infarction (type of heart attack) who received an appropriate care bundle from the trust during the reporting period.
- Care of Patients in Cardiac Arrest In patients who suffer an out of hospital cardiac arrest the delivery of early access, early CPR, early defibrillation and early advanced cardiac life support is vital to reduce the proportion of patients who die from cardiac arrest.
STEMI (ST- elevation myocardial infarction)
This is a type of heart attack. It is important that these patients receive:
- Aspirin – this is important as it can help reduce blood clots forming.
- Glyceryl Trinitrate (GTN) – this is a drug that increases blood flow through the blood vessels within the heart. (Improving the oxygen supply to the heart muscle and also reducing pain).
- Pain scores – so that we can assess whether the pain killers given have reduced the pain.
- Morphine – a strong pain killer which would usually be the drug of choice for heart attack patients.
- Analgesia – Sometimes if morphine cannot be given Entonox, a type of gas often given in childbirth, is used.
The Care Bundle requires each patient to receive each of the above. In addition to the care bundle the Trust measures 999 Call to catheter insertion by the mean and 90th percentile.
Cardiac Arrest
A cardiac arrest happens when your heart stops pumping blood around your body. If someone suddenly collapses, is not breathing normally and is unresponsive, they are in cardiac arrest. The AQI includes:
- Number of cardiac arrests
- ROSC (return of spontaneous circulation) on arrival at Hospital
- Survival to discharge from hospital
- Post Resuscitation care bundle
ROSC and Survival to discharge from hospital are reported within two different groups
- Overall Group
- Resuscitation has commenced in cardiac arrest patients
- Comparator Group
Resuscitation has commenced in cardiac arrest patients AND
- The initial rhythm that is recorded is Ventricular Fibrillation (VF) / Ventricular Tachycardia (VT) i.e., the rhythm is shockable AND
- The cardiac arrest has been witnessed by a bystander AND
- The reason for cardiac arrest is of cardiac origin i.e., it is not a drowning or trauma cause In this element, we would expect a higher performance than the first group.
Post Resuscitation Care Bundle
- 12 lead ECG taken post-ROSC
- Blood glucose recorded?
- End-tidal CO2 recorded?
- Oxygen administered?
- Blood pressure recorded?
- Fluids administration commenced?
Older Adult Fallers discharged at scene
Patients aged 65 years and over who have a fall from below 2 metres should receive a thorough examination to exclude missed injuries before being discharged at scene.
- Detailed physical examination documented?
- History of falls recorded?
- Description of events preceding fall recorded?
- 12 lead ECG assessment documented?
- Postural Hypotension has been assessed?
Care bundles include a collection of interventions that when applied together can help to improve the outcome for the patient.
Year-to-date Clinical Performance AQI’s
Percentages based on data available as of 25 March 2025 for West Midlands Ambulance Service compared to the national average.
| Ambulance Quality Indicators | 2020 to 2021 | 2021 to 2022 | 2022 to 2023 | 2023 to 2024 | 2024 to 2025 | Last national average |
|---|---|---|---|---|---|---|
| STEMI Care Bundle | 95.56% | 86.80% | 77.45% | 95.97% | 95.62% | 78.27% |
| Cardiac Arrest – ROSC At Hospital (Overall Group) | 25.12% | 25.92% | 26.56% | 25.54% | 25.75% | 28.13% |
| Cardiac Arrest – ROSC At Hospital (Comparator) | 44.34% | 44.08% | 46.17% | 47.40% | 47.17% | 53.30% |
| Cardiac Arrest – Survival to Hospital Discharge (Overall) | 8.15% | 8.42% | 6.85% | 6.50% | 8.04% | 9.68% |
| Cardiac Arrest – Survival to Hospital Discharge (Comparator) | 22.26% | 25.93% | 24.20% | 25.00% | 30.23% | 28.10% |
| Post Resuscitation | 69.68% | 66.90% | 68.72% | 65.67% | 82.68% | 82.14% |
| Older Adult Fallers Discharged at scene | No data | No data | No data | No data | 43.75% | 44.19% |
Financial Performance Overview
The Trust met all of its financial targets for 2024 to 2025. This was a significant achievement, against a backdrop of increased service delivery pressures across the NHS including unprecedented levels of hospital handover delays.
The Trust delivered financial efficiencies of £21.3m against a target for the year of £19.7m.
The Trust’s total expenditure for the year was £456m of which £353m (77%) related to paramedic and other salary and employment costs. Non pay expenditure, including costs of operating the ambulance fleet, totalled £103m (23%).
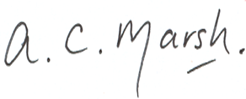
Total capital expenditure for the year was £25m and the Trust met the requirement to manage capital costs within its funded limit.
Income and expenditure
The outturn for 2024 to 2025 reported within the Trust’s accounts was a surplus of £10k. This position is adjusted for a number of technical items for reporting purposes within the Black Country Integrated Care System. The adjusted position was a surplus of £2.648m.
| Income and expenditure | Notes | Plan £000s | Actual £000s | Variance £000s |
|---|---|---|---|---|
| Trust position | 1 | (1,360) | 10 | 1,370 |
| System adjustments | 2 | 63 | 2,638 | 2,575 |
| Adjusted position | 3 | (1,297) | 2,648 | 3,945 |
Note 1 – Trust position
The Trust reported an income & expenditure surplus of £10k for 2024 to 2025 against a planned deficit of £1.36m. The Trust’s position was thus £1.37m better than plan.
Note 2 – System adjustments
The Trust is one of the constituent organisations within the Black Country Integrated Care system (ICS) and as such, the Trust’s financial position is reported within the ICS financial position for 2024 to 2025.
Certain nationally prescribed technical adjustments are applied to the Trust’s position for the purposes of consolidation at ICS level.
The value of technical adjustments for 2024 to 2025 was £2.638m. The majority of this is due to the impairment (reduction in asset carrying value) of the Trust’s headquarters building. The adjustment arose from the NHS five-yearly revaluation exercise which reflects a reduction in value for this type or premises asset.
Note 3 – Adjusted position
After allowing for the technical adjustments, the Trust’s position as included within the Black Country ICS aggregated position for 2024 to 2025 was a surplus of £2.648m
Capital Expenditure
The Trust’s spent £24.998m replacing fleet and other assets during 2024 to2025. Of this total, £1.029m was grant funded and a further £0.418m was financed via net book value of disposals adjustments. This left a net charge against NHS capital allocation funding of £23.551m.
| Capital Funding | £000s |
|---|---|
| Black Country System Allocation | 22,617 |
| National Funding allocation | 936 |
| Total Funding | 23,553 |
| Capital Expenditure | £000s |
|---|---|
| Expenditure | 24,998 |
| Less Grant funded | -1,029 |
| Less net book value of disposals | -418 |
| Charges against funding allocations | 23,551 |
| Net surplus/(decifit) | 2 |
The majority (76%) of the Trust’s capital expenditure was on the replacement programme for ambulances and other fleet assets.
NHS organisations are required to account for leased assets using the IFRS16 accounting standard. Under this standard, leases are capitalised as right-of-use assets, the cost of which creates a charge against capital funding allocations. These charges are included within the expenditure values provided above.
The table shows the value of expenditure charged against capital broken down into leased and purchased assets.
| Charges against Capital Allocations | Lease £000s | Purchase £000s | Total £000s |
|---|---|---|---|
| Ambulances and other vehicles | 10,831 | 8,143 | 18,974 |
| IT equipment | 947 | 2,411 | 3,358 |
| Estates and property | 106 | 2,560 | 2,666 |
| Totals | 11,884 | 13,114 | 24,998 |
| % of total | 48% | 52% | 100% |
Cost Improvement & Efficiencies
The Trust set a cost efficiency plan for 2024 to 2025 of £19.7m. The Trust delivered efficiencies of £21.3m.
The majority of the efficiencies related to productivity improvements within operational areas, and procurement savings against key contracts.
Further details of Trust’s risk profile
The Board Assurance Framework (BAF) is designed to assist the Trust in the control of risk. The Framework incorporates and provides a comprehensive evidence base of compliance against a raft of internal and external standards, targets and requirements.
It is impossible to eliminate all risks and every organisation has to accept a degree of risk. It is for the Board of Directors to decide the balance between mitigating, tolerating and accepting risk which is not mitigated. The Trust Risk Appetite Statement is continually reviewed to ensure a continued progression towards the Trust risk maturity, this includes dynamic updates as the ever-changing healthcare landscape impacts the appetite. The statement sets out the Board’s strategic approach to risk-taking by defining its overall risk appetite, its boundaries, risk tolerance, acceptance and threats to its Strategic Objectives and supports delivery of the Trust’s Risk Management Strategy and Policy.
The committee structure ensures that any new or emerging risks are identified and discussed at meetings and escalated where necessary. Where risks are discussed, the relevant assurance is provided by the subject matter expert in attendance and evidence is provided of action in place. If required, there will be an action added to the minutes and shared with the committee to provide an update at the following meeting. Any new or emerging risks will be added to the Chair’s report to the Executive Management Board for further scrutiny and decision on whether evidence suggests that further work is required, this will be based on the risk appetite of the Trust.
Environmental Matters and the Green Agenda
Task force on climate-related financial disclosures (TFCD)
The Group Accounting Manual (GAM) has adopted a phased approach to implementing the TCFD recommended disclosures as part of the sustainability reporting requirements for NHS bodies. This stems from HM Treasury’s TCFD aligned disclosure guidance for public sector annual reports. These disclosures, as interpreted and adapted for the public sector by HM Treasury, will be phased into sustainability reporting requirements up to the 2025 to 2026 financial year.
Governance
Board oversight of climate-related risks and opportunities
The Board of Directors holds ultimate responsibility for overseeing climate-related risks and opportunities. In January 2022, the Board approved the Trust’s strategic response to these issues through the adoption of the Green Plan, and it receives annual progress reports on its implementation. Climate-related risks, including those associated with funding the Green Plan and deploying suitable technology to support a zero-carbon ambulance service, are captured in the Trust’s Board Assurance Framework. A designated Board member—the Director of Finance—acts as the executive lead for Net Zero Carbon and Climate along with oversight by a nominated Non-Executive Director on the Board, responsible for providing assurance to the Board and escalating relevant risks.
Management’s role in assessing and managing climate-related risks and opportunities
While the Board retains overall responsibility, it has delegated the day-to-day assessment and management of climate-related risks and opportunities to operational management. The Trust has appointed a Sustainability Manager to provide subject matter expertise in identifying, assessing, and responding to these risks and opportunities.
Figure 1 outlines the governance structure supporting climate-related risk management. The Health, Safety & Risk Group, comprising managers from key departments, is responsible for monitoring the Green Plan and driving progress toward the Trust’s net zero carbon objectives. This group also escalates climate-related risks and issues to the Executive Management Board and the Quality Governance Committee.
The organisation has an established Financial Investment Group which manages the key investments of the Trust, including Fleet, Estates, Sustainability and IT capital and revenue investments each year, to deliver on the key strategies of the Trust.
The Quality Governance Committee receives annual reports assessing climate-related risks
and opportunities and monitors progress. The Finance and Performance Committee monitors the delivery of the Trust’s Strategies and reports to the Board on this progress.
RISK MANAGEMENT
Processes for identifying and assessing climate-related risks
The Trust’s process for identifying risks is embedded within its overarching Risk Management Policy of the Trust. Managers are individually responsible for identifying risks that may impact their teams. The Trust has an electronic risk management system.
The Trust makes investment decisions based on the opportunities which arise within the Fleet and Estates strategies and business cases are reviewed by the Financial Investment Group to ensure that the capital investments are assisting in the delivery of strategies including the reduction in carbon emissions.
The Trust has an electronic Sustainability Application. This was developed for the Trust and allows the Sustainability Manager to record and track the effect of Scope 1 and Scope 2 carbon emissions targets set out in the NHS Green Plan. This information informs the key investments the Trust is making in regard to carbon emission reduction and the key actions being taken operationally across the Trust.
To ensure ongoing awareness, the Trust receives monthly updates on relevant environmental legislation, which may introduce new climate-related risks or opportunities.
Environmental incidents are captured through the Trust’s Incident Reporting System (IRS) The Sustainability Manager and Health, Safety and Risk Team review these reports. Where necessary, incidents are reassigned to appropriate managers and investigated through an After Action Review, potentially identifying further risks.
Climate-related risks may also surface through existing governance forums or committee discussions.
The Trust’s Emergency Preparedness, Resilience and Response (EPRR) programme requires managers to consider climate-related risks within their business continuity planning.
Processes for managing climate-related risks
The Trust manages identified risks through a structured risk register process. Risks requiring active management are added to a relevant register, with responsibility for each risk assigned to a manager whose objectives are impacted. Each risk is assessed and scored using a standard matrix based on likelihood and impact (scored 1–5, with a maximum risk score of 25). All risks must include current controls and planned mitigation actions aimed at reducing the overall risk score where possible.
Risk registers are actively maintained and reviewed across the organisation. Oversight responsibility lies with the appropriate director. Risk registers are collated and reviewed with regular reporting and challenge occurring at relevant committees. Risks scoring 12 or above are subject to specific scrutiny and discussion as part of this assurance process.
The Emergency Preparedness, Resilience and Response (EPRR) Risk Register addresses adaptation risks, such as those posed by extreme weather events (e.g., flooding, heatwaves) and long-term climate change. These risks are considered enduring and, given the Trust’s limited ability to influence their root causes, are managed through preparedness and business continuity measures.
Additionally, the risk register is used to capture specific climate-related risks affecting individual sites or departments—for example, locations identified as particularly vulnerable to flooding. The Trust is developing further processes to mitigate these known risks and has undertaken geographic mapping of flood-prone areas as part of this work.
At present, the Trust does not apply external risk assessment frameworks specifically designed for climate-related risks but continues to evolve its internal processes to strengthen climate risk management.
Processes for identifying, assessing, and managing climate-related risks are integrated into the organisations overall risk management
The Trust plans to integrate in climate-related risks into its overall risk management framework in 2025 to 2026, as outlined in its Risk Management Policy. Climate-related risks are identified, assessed, and managed using the same processes applied to all organisational risks. This includes scoring risks based on likelihood and impact, assigning ownership, and reviewing them through regular governance channels.
The Trust’s sustainability manager attends meetings at ICB and National level which provides the trust with majority of intelligence and information on this subject in the NHS. Information arising from these meetings is then used to inform the Trust’s and plan and priorities.
METRICS AND TARGETS
Metrics used to assess climate-related risks and opportunities in line with its strategy and risk management approach
The Trust monitors key climate-related metrics through a dedicated dashboard report, which supports the assessment of risks and opportunities in line with its sustainability strategy and risk management approach. The dashboard includes the following core indicators:
- Energy consumption: To monitor usage trends and identify opportunities for efficiency improvements.
- Volume of waste: To track waste generation and support reduction initiatives.
- Carbon footprint: Covering Scope 1, Scope 2, and a subset of Scope 3 emissions, providing insight into direct and indirect emissions associated with the Trust’s operations.
These metrics are reviewed regularly to inform decision-making, monitor progress toward Net Zero targets, and support the identification and management of climate-related risks and opportunities.
Scope 1, Scope 2, and Scope 3 greenhouse gas (GHG) emissions disclosures and related risks
The Trust discloses its Scope 1, Scope 2, and a subset of Scope 3 greenhouse gas (GHG) emissions in its Green Plan. These emissions are calculated annually to monitor progress toward the Trust’s Net Zero targets.
- Scope 1 includes direct emissions from sources owned or controlled by the Trust, such as fleet vehicles and on-site gas consumption.
- Scope 2 includes indirect emissions from purchased electricity.
- Scope 3 includes selected indirect emissions, such as waste disposal, but is yet to incorporate business travel and some elements of the supply chain.
These emissions represent both a reputational and operational risk to the Trust. For example, rising energy costs, increased regulatory requirements, and the transition to low-carbon technologies all present potential challenges. Understanding and reducing these emissions is critical to managing climate-related risks and aligning with national Net Zero commitments.
Full emissions data and methodologies are detailed in the Green Plan.
Targets used to manage climate-related risks and opportunities and performance against targets
The Trust has established clear targets to manage climate-related risks and opportunities, aligned with national NHS Net Zero commitments. These include:
- Achieving Net Zero carbon emissions for direct (Scope 1 and 2) emissions by 2040, and
- Achieving Net Zero for indirect (Scope 3) emissions by 2045.
Performance against these targets is reviewed regularly through the Trust’s carbon reporting dashboard and periodically reported to committees. This enables early identification of deviations from the emissions trajectory and supports timely mitigation action.
Planned Improvements in 2025 to 2026
The Trust provided an update to the Board in April 2025 on the current sustainability progress arising and from that the Trust will update the Green Plan and present it to the Board for approval in May 2025. There is a plan to implement a dedicated multidisciplinary meeting chaired by the accountable director on a regular basis. This meeting will create a more formal structure to manage and plan the Trust’s response to sustainability and climate change matters. This meeting will report to one of the Trust’s formal committees.
Carbon Reduction
The Trust has undertaken risk assessments and has plans in place which take account of the “delivering a Net Zero Health service” report under the Greener NHS Programme. The Trust ensures the Climate Change Act and Adaptation Reporting requirements are complied with.
Progress on delivery of the Green Plan
The Board at its meeting in January 2022 approved the Trust’s WMAS Green Plan 2022 to 2026. There is requirement for all Trusts to have a Green Plan which provides a structured way for each Trust and ICS to set out the carbon reduction initiatives that are already underway and their plans for the subsequent years. Its introduction includes the following: Over the last 10 years, the NHS has taken notable steps to reduce its impact on climate change. As the biggest employer in this country, there is more that the NHS can do. Action must not only cut NHS emissions, currently equivalent to 4% of England’s total carbon footprint, but also build adaptive capacity and resilience into the way care is provided.
WMAS have led the way in the ambulance service implementing a large amount of change to our operation which has led to significant reductions in our direct and indirect carbon footprint, including:
- Implementing the Make Ready Model – reducing the estate portfolio by Commissioning new build sites compliant with the exacting requirements in the BREEAM (Building Research Establishment Environmental Assessment Methodology) standards.
- Changing our lighting on sites to LED lighting reducing a significant amount of electricity usage.
- Delivering a fleet replacement programme with no front-line operational vehicles over 5 years old – WMAS now operate the most modern ambulance fleet in the country which is compliant to the latest euro emission standards.
West Midlands Ambulance Service University NHS Foundation Trust is committed to the ongoing protection of the environment through the development of a sustainable strategy. Sustainability is often defined as meeting the needs of today without compromising the needs of tomorrow.
A sustainable health and care system is achieved by delivering high quality care and improved public health without exhausting natural resources or causing severe ecological damage.
The approved Green Plan sets out the Trust’s commitment to ensure governance and management arrangements are in place to deliver both the Trust’s statutory responsibilities for sustainability and to achieve the target set by the NHS of reducing its carbon footprint set out in “Delivering a Net ZERO National Health Service (published October 2020). The Green Plan is available for inspection
Carbon Reduction
The Trust has undertaken risk assessments and has plans in place which take account of the “delivering a Net Zero Health service” report under the Greener NHS Programme. The Trust ensures the Climate Change Act and Adaptation Reporting requirements are complied with.
Progress on delivery of the Green Plan
The Board at its meeting in January 2022 approved the Trust’s WMAS Green Plan 2022 to 2026. There is requirement for all Trusts to have a Green Plan which provides a structured way for each Trust and ICS to set out the carbon reduction initiatives that are already underway and their plans for the subsequent years. Its introduction includes the following: Over the last 10 years, the NHS has taken notable steps to reduce its impact on climate change. As the biggest employer in this country, there is more that the NHS can do. Action must not only cut NHS emissions, currently equivalent to 4% of England’s total carbon footprint, but also build adaptive capacity and resilience into the way care is provided.
WMAS have led the way in the ambulance service implementing a large amount of change to our operation which has led to significant reductions in our direct and indirect carbon footprint, including:
- Implementing the Make Ready Model – reducing the estate portfolio by Commissioning new build sites compliant with the exacting requirements in the BREEAM (Building Research Establishment Environmental Assessment Methodology) standards.
- Changing our lighting on sites to LED lighting reducing a significant amount of electricity usage.
- Delivering a fleet replacement programme with no front-line operational vehicles over 5 years old – WMAS now operate the most modern ambulance fleet in the country which is compliant to the latest euro emission standards.
West Midlands Ambulance Service University NHS Foundation Trust is committed to the ongoing protection of the environment through the development of a sustainable strategy. Sustainability is often defined as meeting the needs of today without compromising the needs of tomorrow.
A sustainable health and care system is achieved by delivering high quality care and improved public health without exhausting natural resources or causing severe ecological damage.
The approved Green Plan sets out the Trust’s commitment to ensure governance and management arrangements are in place to deliver both the Trust’s statutory responsibilities for sustainability and to achieve the target set by the NHS of reducing its carbon footprint set out in “Delivering a Net ZERO National Health Service (published October 2020). The Green Plan is available for inspection
Tacking Health Inequalities
Public Sector Equality Duty Compliance Annual Equality Report
The Trust published its Annual Equality Report in July 2024 which encompassed the progress made in relation to Equality and Diversity and how the Trust had complied with the Public Sector Equality Duty under the Equality Act 2010.
Incorporated within the report was the Data Analysis report 2024 to ensure that the Specific Duties had been adhered to. The Trust reported on the Equality Objectives that had been established in the Equality Strategy as required under the duty.
The Annual Equality Report provides information on progress to enable the Trust to make informed decisions and incorporate the data into future plans and ensure equality across all Protected Characteristics.
The 2024 Diversity and Inclusion Annual Report can be found on the Trust website when it was published in the summer of 2024.
Equality Delivery System 3
‘Everyone counts’ is a key principle that applies to everyone served by the NHS and is at the heart of the NHS Constitution.
The main purpose of the Equality Delivery System is to help local NHS organisations, in discussion with local partners including local people, review and improve their performance for people with characteristics protected by the Equality Act 2010. By using the Equality Delivery System 3 (EDS3), NHS organisations can also be helped to deliver on the Public Sector Equality Duty (PSED).
The Equality Delivery System provides a way for the organisation to show how it is doing against the three domains (they are called goals in the EDS2 framework). The EDS Technical Guidance document is available at: https://future.nhs.uk/EHIME/view?objectID=119804773
All NHS organisations are expected to use the system to help them improve their equality performance for patients, communities and staff, as well as help them to meet the requirements of the Public Sector Equality Duty.
The Trust adopted the EDS3 2022 framework which comprised of 11 specific outcomes that are grouped across the following three domains:
Domain 1. Commissioned or Provided Services. Focus – Patient access and experience, reducing inequalities and enabling better health outcomes.
Domain 2. Workforce Health and Wellbeing. Focus – Ensuring that all workforce members are fully supported in relation to health and wellbeing.
Domain 3. Inclusive Leadership. Focus – How leadership demonstrates a commitment to equality and how it works in a way that identifies equality issues and manages them.
Each domain has outcomes that are evaluated and scored against set criteria, and experiences of stakeholders. These ratings provide assurance and/or direction for further improvement. For 2024, WMAS has completed the EDS framework and created an action plan, which can be accessed on the Trust website.
Social, community, anti-bribery and human rights issues
The geographical and demographic spread of the region served by the West Midlands Ambulance Service means that issues of diversity and inclusion are fundamental, yet also challenging, to the successful achievement of the Trust’s strategic objectives as well as addressing health inequalities. There are clear health inequalities between areas, with indicators showing lower levels of health tending to be clustered in the metropolitan and urban areas and the Trust continues to work with UK Health Security Agency (formerly Public Health England), Integrated Care Systems and the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) to identify and address them. Through regular engagement and education, the Trust will work to improve accessibility and, where necessary, the quality of services for population groups to assist in reducing these inequalities. The Trust has action plans in place which are working towards creating a workforce which is representative of the population that WMAS serves.
Signed
Position: Chief Executive, Date: 23 June 2025
Accountability Report
Directors’ Report
Board members during the financial year
The Board of Directors serving during 2024 to 2025 (1 April 2024 to 31 March 2025)
Voting Members of the Board of Directors
Professor Ian Cumming, Chairman
Anthony Marsh, Chief Executive Officer
Alexandra Hopkins, Non-Executive Director
Mohammed Fessal, Non-Executive Director
Narinder Kaur Kooner (to 4.11.24), Non-Executive Director
Mushtaq Khan, Non-Executive Director
Sukhjeeven Nat (from 5.11.24), Non-Executive Director
Julie Jasper, Non-Executive Director
Suzanne Banks, Non-Executive Director
Karen Rutter, Director of Finance
Dr Alison Walker (to 30.11.24), Medical Director
Dr Richard Steyn (from 1.12.24), Medical Director
Caron Eyre, Director of Nursing
Nathan Hudson, Director of Performance an Improvement.
Carla Beechey, Director of People.
Non-Voting Members of the Board of Directors
Murray MacGregor, Communications Director
Vivek Khashu, Strategy and Engagement Director
Nick Henry, Paramedic Practice and Patient Safety Director
Register of interests
The Trust maintains a Register of Interests for the Board of Directors and the Council of Governors that is open to the public. The register is reviewed by the Audit Committee.
The register is available for inspection on the Trust’s website – Declarations – West Midlands Ambulance Service University NHS Foundation Trust
Better Payment Practice Code
The Trust is committed to applying the Better Payment Practice Code (BPPC) to the payment of creditors. In line with most NHS bodies the Trust seeks to pay 95% of all NHS and non-NHS trade payables within 30 days of receipt of the goods or a valid invoice. The Trust measures achievement in terms of both the number and value of invoices. Commitment to this standard is embedded in the Trust’s terms and conditions of contracting for the provision of goods and services. The Trust fully achieved the public sector payments targets in 2024 to 25.
The Trust’s performance is summarised in the table below:
| Invoices | Total number of invoices | Number of invoices paid within 30 days | % of invoices paid within 30 days |
|---|---|---|---|
| Total | 23,579 | 23,118 | 98.0% |
| Non-NHS | 22,333 | 21,899 | 98.1% |
| NHS | 1,246 | 1,219 | 97.8% |
| Invoices | Total value of invoices £000 | Value of invoices paid within 30 days £000 | % of invoices paid within 30 days |
|---|---|---|---|
| Total | 189,370 | 187,078 | 98.8% |
| Non-NHS | 180,837 | 178,689 | 98.8% |
| NHS | 8,533 | 8,389 | 98.3% |
Care Quality Commission (CQC) and NHS England, Well-led Framework Disclosures
As detailed in the Annual Governance Statement, arrangements are in place within the Trust to assure the Board of Directors and stakeholders that quality governance arrangements suitably scrutinise the quality of the organisation and present a balanced view of the organisation.
To provide high-quality, person-centred care for all the Trust is committed to be a high performing organisation working in partnership with, and for, local people and communities.
The Trust has a robust governance framework for quality. This provides assurance that the essential standards of quality and safety are being delivered and the processes for the governance of quality are embedded throughout the organisation.
The Trust’s Medical Director and Director of Nursing advise the Board on clinical issues and the Paramedic Practice and Patient Safety Director has responsibility for Professional Paramedic practice, Patient Safety, Learning from deaths, Clinical and serious incident investigations and Duty of Candour.
The Trust also has a Non-Executive Director with clinical experience who Chairs the Quality Governance Committee and works closely with the Executive leads.
The Trust’s Quality Governance Committee (QGC) provides assurance to the Board on clinical standards and registration compliance requirements. The Committee’s primary responsibility is to monitor and review quality and clinical aspects of performance.
The Committee ensure required standards are achieved and action taken where required and that the organisations systems and processes in relation to quality are robust and well-embedded so that priority is given within the organisation, to identifying and managing risks to the quality of care.
There is a schedule of business that includes appropriate review of nationally and regionally agreed quality performance measurements such as Ambulance Quality Indicators (AQIs) relating to aspects of clinical care, workforce data, patient and staff feedback and timeliness of operational response targets.
Fees and charges (income generation)
Income disclosures
Section 43(2A) of the NHS Act 2006 (as amended by the Health and Social Care Act 2012) requires that the income from the provision of goods and services for the purposes of the health service in England must be greater than its income from the provision of goods and services for any other purposes.
The Trust confirms that it is compliant with this restriction.
The Trust furthermore discloses, as required by S43(3A) of the NHS Act 2006, that the Trust received a total of £571,550 for the provision of crew hire to commercial events for which a commercial rate was charged. This included shows and sporting events and the net contribution from these services was used to support the provision of health services.
Remuneration Report
The remuneration report provides information on those persons in senior positions having authority or responsibility for directing or controlling the major activities of the Trust.
Annual statement on remuneration
The Trust’s Remuneration and Nominations Committee (the Committee) manages the appointment of Executive Directors and agrees their remuneration, allowances and terms of service.
The Committee does not determine the terms and conditions of office of the Chair and Non-Executive Directors. These are determined by the Council of Governors.
The Committee Chair conducts the Chief Executive’s appraisal and appraises the Non-Executive Directors within a framework agreed by the Council of Governors and NHSE. The Chief Executive appraises the other Executive Directors.
In determining whether to pay an annual bonus to the CEO the Committee takes account of the Chief Executive’s performance against personal and corporate objectives to ensure performance conditions are met.
When determining remuneration, the Committee is sensitive to overall financial pressures, pay and employment conditions elsewhere in the Trust, other NHS Foundation Trusts and comparable organisations both regionally and nationally.
During the year, and at the request of the Chair, advice was provided to the Committee by the Chief Executive and Director of People. Advice is also provided, where appropriate and required, from Mills and Reeve LLP, the Trust’s Legal Advisor and Head of Claims and Coroners. In its deliberations the Committee takes account of national advice to ensure all decisions are defensible and equitable and takes advice from external professional bodies if required.
During the year ended 31 March 2025 the members of the Committee were the Non-Executive Directors and the Chief Executive (who was not in attendance when discussing his remuneration). Professor Ian Cumming was Chairman. During 2024 to 2025 the Remuneration and Nominations Committee met on the following occasions: 29 May 2024, 14 October 2024 and 26 February 2025.
The Chief Executive and Executive Directors are directly employed by the Trust on contracts with a notice period of six months pro-rata with the exception of the Medical Director who is engaged on a secondment basis from his employing Hospital Trust.
None of the Trust’s Executive Directors received a performance related element to their pay in 2024 to 2025 with the exception of the Chief Executive Officer.
Senior managers’ remuneration policy
Since the inception of the Trust as an NHS Foundation Trust on 1 January 2013, Executive Directors have been remunerated under a contract that mirrors the Very Senior Managers Pay Framework with a single point personal salary. The Trust complies with the NHSE Very Senior Managers pay framework.
Executive Director salary is determined by the Remuneration and Nominations Committee, who review salary levels regularly by considering benchmarking data to ensure they remain competitive.
The Committee has adopted the NHSE Guidance on pay for very senior managers in NHS trusts and foundation trusts, as its policy on matters relating to remuneration and other matters within its terms of reference.
The Remuneration and Nominations Committee considers the pay and benefits of all Executive Directors on the VSM pay framework.
The Chief Executive Officer considers the performance of each Executive Director against the specific objectives set for them for the year, and the Chairman further considers under grandparent rights, the achievements of each Director.
There is no Performance Related Pay (PRP) process utilised by the Trust for Senior Managers or Executive Directors.
Pay uplifts are based on the recommendations of the Senior Salaries Review Body (SSRB) published each year. The only exception to this approach is in the remuneration of the Chief Executive Officer, where there is a performance related pay scheme in place.
Each year the Chief Executive Officer’s performance is considered against criteria on which up to a 10% PRP payment (capped at £17,500) can be awarded based on successful achievement of key strategic objectives. Any Award is non-pensionable.
The PRP Scheme assesses the performance of the Chief Executive Officer in line with the Trust’s objective setting and performance appraisal process and the CEO is marked as either A (Exceeds Expectations), B (Meets Expectations), C (Fails to Meet Expectations).
Annual report on remuneration
Remuneration and Nominations Committee
Committee membership and attendance below.
| Name | Title | 29.5.24 | 14.10.24 | 26.2.25 |
|---|---|---|---|---|
| Ian Cumming | Chairman (NED) | Attended | Attended | Attended |
| Anthony Marsh | CEO | Attended | Attended | Attended |
| Professor Hopkins | NED | Attended | Attended | Apology |
| Suzanne Banks | NED | Attended | Attended | Attended |
| Carla Beechey | Director of People and HR advisor to the Committee | Attended | Attended | Attended |
| Mohammed Fessal | NED | Attended | Attended | Attended |
| Julie Jasper | NED | Attended | Attended | Attended |
| Mushtaq Khan | NED | ✔ | ✔ | ✔ |
| Narinder Kooner(to 4.11.24) | NED | ✔ | ✔ | Had left the Trust |
| Sukhjeeven Nat (From 5.11.24) | NED | Had not joined Trust | Had not joined Trust | Apology |
The only remuneration changes were the national cost of living increase agreed by the independent body which was awarded to both Executive and Non-Executive Directors otherwise no other changes. The Committee reviewed and made an award to the CEO under the approved bonus scheme.
Disclosures relating to specific pay and remuneration matters
Directors’ Salaries and Allowances (subject to audit)
Single total figure table – April 2024 – March 2025
| Name and title | Salary (bands of £5,000) £’000 | Expense Payments (taxable)to nearest £100 | Performance pay and bonuses (bands of £5,000)£’000 | Long Term Performance pay and bonuses (bands of £5,000)£’000 | All Pension related benefits (bands of £2,500)£’000 | Total (bands of £5,000) £’000 |
|---|---|---|---|---|---|---|
| Mr A C Marsh, Chief Executive | 235-240 | 0 | 15-20 | 0 | 0 | 255-260 |
| Mrs Karen Rutter1 Director of Finance | 140-145 | 5 | 0 | 0 | 27.5-30.0 | 170-175 |
| Dr Alison Walker, Medical Director (to 30.11.24) | 95-100 | 0 | 0 | 0 | 0 | 95-100 |
| Dr Richard SteynInterim Medical Director (from 1.12.24) | 70-75 | 0 | 0 | 0 | 0 | 70-75 |
| Mrs Caron EyreDirector of Nursing (from 23.8.23) | 50-55 | 0 | 0 | 0 | 0 | 50-55 |
| Mr Nathan HudsonDirector of Performance and Improvement | 145-150 | 0 | 0 | 0 | 75-77.5 | 220-225 |
| Mrs Carla BeecheyDirector of People | 130-135 | 1 | 0 | 0 | 80-82.5 | 210-215 |
| Professor Ian CummingChairman | 60-65 | 0 | 0 | 0 | 0 | 60-65 |
| Mrs Alexandra HopkinsNon-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mr Sukhjeeven Nat (from 5.11.24) | 5-10 | 0 | 0 | 0 | 0 | 5-10 |
| Mrs Julie Jasper, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mrs Narinder Kooner, Non-Executive Director (to 4.11.24) | 5-10 | 0 | 0 | 0 | 0 | 5-10 |
| Mr Mushtaq Ahmed- Khan, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mr Mohammed Fessal, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mrs Suzanne Banks, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
April 2023 – March 2024
| Name and title | Salary (bands of £5,000) £’000 | Expense Payments (taxable) to nearest £100 | Performance pay and bonuses (bands of £5,000)£’000 | Long Term Performance pay and bonuses (bands of £5,000)£’000 | All Pension related benefits (bands of £2,500)£’000 | Total (bands of £5,000) £’000 |
|---|---|---|---|---|---|---|
| Mr A C Marsh, Chief Executive | 225-230 | 0 | 15-20 | 0 | 0 | 240-245 |
| Mrs Karen Rutter Director of Finance | 125-130 | 0 | 0 | 0 | 697.5-700 | 820-825 |
| Dr Alison Walker, Medical Director (to 30.11.24) | 145-150 | 0 | 0 | 0 | 0 | 145-150 |
| Dr Richard SteynInterim Medical Director (from 1.12.24) | 80-85 | 0 | 0 | 0 | 0 | 80-85 |
| Mrs Caron EyreDirector of Nursing (from 23.8.23) | 30-35 | 0 | 0 | 0 | 0-2.5 | 30-35 |
| Mr Nathan HudsonDirector of Performance and Improvement | 50-55 | 0 | 0 | 0 | 87.5-90 | 135-140 |
| Mrs Carla BeecheyDirector of People | 20-25 | 54 | 0 | 0 | 0 | 25-30 |
| Professor Ian CummingChairman | 60-65 | 0 | 0 | 0 | 0 | 60-65 |
| Mrs Alexandra HopkinsNon-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mrs Julie Jasper, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mrs Narinder Kooner, Non-Executive Director (to 4.11.24) | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mr Mushtaq Ahmed- Khan, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
| Mr Mohammed Fessal, Non-Executive Director | 15-20 | 0 | 0 | 0 | 0 | 15-20 |
Notes
Pension figures provided by the NHS Pensions Agency with further clarification on accuracy to be provided.
This note relates only to those senior managers with a voting right on the Trust’s Board of Directors. The expense payments are for lease cars.
The clinical element of the remuneration of Dr A Walker as Medical Director and Dr R Steyn as Interim Medical Director was £0.
Pension entitlements (subject to audit)
| Name and title | Real increase in pension at age 60 (bands of £2,500) £’000 | Real increase in pension lump sum at aged 60 (bands of £2,500) £’000 | Total accrued pension at age 60 at 31 March 2025 (bands of £5,000) £’000 | Lump sum at pension age 60 related to accrued pension at 31 March 2025 (bands of £5,000) £’000 | Cash Equivalent Transfer Value at 1 April 2024 £’000 | Real increase in Cash Equivalent Transfer Value £’000 | Cash Equivalent Transfer Value at 31 March 2025 £’000 | Employer’s contribution to stakeholder pension To nearest £’000 |
|---|---|---|---|---|---|---|---|---|
| Mr A C Marsh, Chief Executive | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mrs Karen RutterDirector of Finance | 0-2.5 | 0 | 45-50 | 115-120 | 984 | 34 | 1101 | 0 |
| Nathan Hudson, Director of Performance and Improvement | 2.5-5 | 2.5-5.0 | 50-55 | 135-140 | 1043 | 81 | 1212 | 0 |
| Caron EyreDirector of Nursing2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Dr Alison Walker1 Medical Director (to 30.11.24) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Dr Richard Steyn1, Interim Medical Director(from 1.12.24) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Carla BeecheyDirector of People | 2.5-5 | 0 | 60-65 | 0 | 759 | 61 | 887 | 0 |
Notes
1The pension entitlement for Dr Alison Walker and Dr Richard Steyn is not available due to secondment arrangements.
2The pension value for the Director of Nursing has been disclosed as nil because the calculation resulted in a negative value.
Cash equivalent transfer value (CETV) figures are calculated using the guidance on discount rates for calculating unfunded public service contribution rates that was extant on 31 March 2025. HM Treasury published updated guidance on 27 April 2023; this guidance will be used in the calculation of 2024 to 2025 CETV figures.
Cash Equivalent Transfer Value (CETV) is the actuarially assessed capital value of the pension scheme benefits accrued by a member at a particular point in time. The benefits valued are the member’s accrued benefits and any contingent spouse’s pension payable from the scheme.
A CETV is a payment made by a pension scheme, or arrangement to secure pension benefits in another pension scheme, or arrangement when the member leaves a scheme and chooses to transfer the benefits in their former scheme. The pension figures shown relate to the benefits that the individual has accrued as a consequence of their total membership of the pension scheme. They also include any additional pension benefit accrued to the member as a result of their purchasing additional years of pension service in the scheme at their own cost. CETVs are calculated within the guidelines and framework prescribed by the Institute and Faculty of Actuaries.
Real increase in CETV – This reflects the increase in CETV effectively funded by the employer. It does not include the increase in accrued pension due to inflation, contributions paid by the employee (including the value of any benefits transferred from another pension scheme or arrangement) and uses common market valuation factors for the start and end of the period. CETVs are calculated by the Government Actuary Department (GAD) based on the assumption that benefits are indexed in line with CPI. The last published actuarial valuation undertaken for the NHS Pension Scheme was completed for the year ending 31 March 2020.
NHS Pensions use pension and lump sum data from their systems without any adjustment for a potential future legal remedy required as a result of the McCloud judgment. (This is a legal case concerning age discrimination over the manner in which UK public service pension schemes introduced a Career Average Revalued Earnings (CARE) benefit design in 2015 for all but the oldest members who retained a Final Salary design.). We believe this approach is appropriate given that there is still considerable uncertainty on how the affected benefits within the new NHS 2015 Scheme would be adjusted in future once legal proceedings are completed.
Pension Related Benefits of Single Total Remuneration
The Large and Medium-sized Companies and Groups Regulations require that the Trust includes the value of pension related benefits in the table of Salaries and Allowances. This figure includes those benefits accruing to a director from membership of the NHS Pensions Scheme. Accrued pension benefit balances represent the annual increase in pension entitlement at the end of the financial year and the rate payable at the start of the year.
| Name and title | All Pension related benefits 2024 to 2025 £000s | All Pension related benefits 2023 to 2024 £000s |
|---|---|---|
| Mr A C Marsh, Chief Executive | 0 | 0 |
| Mrs Karen Rutter, Director of Finance | 29.94 | 698.41 |
| Mrs Caron Eyre, Director of Nursing2 | 0 | 1.44 |
| Mr Nathan Hudson, Director of Performance and Improvement | 75.57 | 87.96 |
| Ms Carla Beechey, Director of People | 81.04 | 0 |
| Dr Alison Walker1, Medical Director (to 30.11.24) | 0 | 0 |
| Dr Richard Steyn1, Medical Director (from 1.12.24) | 0 | 0 |
Notes
1The pension entitlement for Dr Alison Walker and Dr Richard Steyn is not available due to secondment arrangements.
2The pension value for the Director of Nursing has been disclosed as nil because the calculation resulted in a negative value.
Payments for loss of office
None.
Payments to past senior managers
None.
Expenses of the Governors and Directors
Reporting bodies are required to disclose the information relating to the expenses of the governors and the directors:
| Period April 2024 to March 2025 | Period April 2023 to March 2024 | |
|---|---|---|
| Number of Governors in Office in the period | 17 | 22 |
| Number of Governors receiving expenses in the period | 7 | 8 |
| Sum of expenses paid to Governors in the period | £2.9 (£’00) | £2.6 (£’00) |
| Number of Directors in office in the period | 15 | 16 |
| Number of Directors receiving expenses | 5 | 5 |
| Sum of expenses paid to Directors in the period | £3.7 (£’00) | £5.1 (£’00) |
Fair Pay Disclosures (subject to audit)
NHS Foundation Trusts are required to disclose the relationship between the remuneration of the highest-paid director in their organisation and the lower quartile, median and upper quartile remuneration of the organisation’s workforce.
The banded remuneration of the highest-paid director in the organisation in the financial year 2024 to 2025 was £285,000 to £290,00 (2023 to 2024, £275,00 to £280,000). This is a change between years of 4.32%.
Total remuneration includes salary, non-consolidated performance-related pay, benefits-in-kind, but not severance payments. It does not include employer pension contributions and the cash equivalent transfer value of pensions.
For employees of the Trust as a whole, the range of remuneration in 2024-25 was from £22,369 to £287,660 (2023 to 2024 £20,576 to £275,747). Zero employees received remuneration in excess of the highest-paid director in 2024 to 2025 (2023 to 2024: zero employees).
The remuneration of the employee at the 25th percentile, median and 75th percentile is set out below. The pay ratio shows the relationship between the total pay and benefits of the highest paid director (excluding pension benefits) and each point in the remuneration range for the organisation’s workforce. The relationship to the remuneration of the organisation’s workforce is disclosed in the below table.
| 2024 to 2025 | 25th percentile | Median | 75th percentile |
|---|---|---|---|
| Total remuneration (£) | £30,599 | £38,196 | £50,830 |
| Salary component of total remuneration (£) | £25,674 | £29,970 | £37,338 |
| Pay ratio information | 9.5:1 | 7.6:1 | 5.7:1 |
2023 to 2024 | 25th percentile | Median | 75th percentile |
|---|---|---|---|
| Total remuneration (£) | £30,438 | £36,881 | £49,474 |
| Salary component of total remuneration (£) | £22,816 | £28,407 | £37,350 |
| Pay ratio information | 9.1:1 | 7.5:1 | 5.6:1 |
The percentage change in average employee remuneration (Note 1) between years is 2.67%. Total remuneration includes salary, non-consolidated performance-related pay, benefits-in kind, but not severance payments. It does not include employer pension contributions and the cash equivalent transfer value of pensions.
Note 1 – based on total for all employees on an annualised basis divided by full-time equivalent number of employees.
Signed
Position Chief Executive, Date 23 June 2025
Staff Report
Analysis of Staff Costs (Subject to audit)
| Category | Permanent £000 | Other £000 | 2024 to 2025 Total £000 | 2023 to 2024 Total £000 |
|---|---|---|---|---|
| Salaries and wages | 272,122 | 166 | 272,288 | 241,124 |
| Social security costs | 25,947 | 0 | 25,947 | 24,529 |
| Apprenticeship levy | 1,350 | 0 | 1,350 | 1,274 |
| Employer’s contributions to NHS pension scheme | 53,587 | 0 | 53,587 | 43,089 |
| Pension cost – other | 0 | 0 | 0 | 0 |
| Other post employment benefits | 0 | 0 | 0 | 0 |
| Other employment benefits | 0 | 0 | 0 | 0 |
| Termination benefits | 0 | 0 | 0 | 0 |
| Temporary staff | 0 | 0 | 0 | 0 |
| Total gross staff costs | 353,006 | 166 | 353,172 | 310,016 |
| Recoveries in respect of seconded staff | 0 | 0 | 0 | 0 |
| Total staff costs | 353,006 | 166 | 353,172 | 310,016 |
| Of which Costs capitalised as part of assets | 0 | 0 | 0 | 0 |
| Average number of employees (WTE basis) (subject to audit) | Permanent Number | Other Number | 2024 to 2025 Total number | 2023 to 2024 Total number |
|---|---|---|---|---|
| Medical and dental | 4 | – | 4 | 4 |
| Ambulance staff | 2,772 | 0 | 2,772 | 2,532 |
| Administration and estates | 578 | 0 | 578 | 585 |
| Healthcare assistants and other support staff | 3,111 | 0 | 3,111 | 3,118 |
| Nursing, midwifery and health visiting staff | 54 | 0 | 54 | 48 |
| Nursing, midwifery and health visiting learners | 0 | 0 | 0 | 0 |
| Scientific, therapeutic and technical staff | 3 | 0 | 3 | 3 |
| Healthcare science staff | 0 | 0 | 0 | 0 |
| Social care staff | 0 | 0 | 0 | 0 |
| Other | 0 | 0 | 0 | 0 |
| Total average numbers | 6,522 | 0 | 6,522 | 6,290 |
Of which: Number of employees (WTE) engaged on capital projects | 0 | 0 | 0 | 0 |
Analysis of Staff Numbers
Contract type breakdown on 31st March 2025
| Contract Type | Bank FTE | Fixed term temp FTE | Perm-anent FTE | Total FTE | Bank Head-count | Fixed term temp Head-count | Perm-anent Head-count | Total Head-count |
|---|---|---|---|---|---|---|---|---|
| Directors (excl. NEDs) | 0.00 | 0.00 | 6.90 | 6.90 | 0 | 0 | 8 | 8 |
| Senior Managers | 0.00 | 0.70 | 11.00 | 11.70 | 0 | 2 | 11 | 13 |
| Employees (excl. Directors and Senior Managers) | 0.00 | 21.17 | 6624.42 | 6645.59 | 39 | 29 | 7174 | 7242 |
| Total | 0.00 | 21.87 | 6642.32 | 6664.19 | 39 | 31 | 7193 | 7263 |
Analysis of Staff by Gender
The Trust has a good mix of male and female staff at all levels within the Trust.
Gender breakdown on 31st March 2025
| Contract type | Female FTE | Male FTE | Total FTE | Female Head-count | Male Head-count | Total Head-count |
|---|---|---|---|---|---|---|
| Directors (excl. NEDs) | 2.4 | 4.5 | 6.9 | 3 | 5 | 8 |
| Senior Managers | 5.6 | 6.1 | 11.7 | 6 | 7 | 13 |
| Employees (excl. Directors and Senior Managers) | 3498.03 | 3147.56 | 6645.59 | 3862 | 3380 | 7242 |
| Total | 3506.03 | 3158.16 | 6664.19 | 3871 | 3392 | 7263 |
Sickness Absences – Sickness absence data
% Sickness Absence Rate FTE (Excluding Covid)
April 2024, 4.19%
May 2024, 4.15%
June 2024, 4.13%
July 2024, 4.60%
August 2024, 4.71%
September 2024, 4.75%
October 2024, 4.69%
November 2024, 5.01%
December 2024, 5.84%
January 2025, 5.27%
February 2025, 4.82%
March 2025, 4.39%
Average for the Year 1 April 2024 to 31 March 2025, 4.72%
Average Absence Days Lost (Full-Time Equivalent) per Full-Time Equivalent January 2024 to December 2024*
Average Full-Time Equivalent of Staff 6473
Total Days Lost Full-Time Equivalent 70364
Average Working Days Lost (FTE) per FTE 10.9
*Note – Department of Health sickness absence figures are reported on a calendar year basis, rather than for the financial year.
Staff policies and actions applied during the financial year
The Trust has a full set of Workforce Policies which are regularly reviewed. These include the Recruitment and Selection Policy, the Sickness Absence Management Policy, the People Strategy, Flexible Working and the Freedom to Speak Up Policy.
The Trust’s Policy Group facilitates work between elected staff representatives and management to ensure the Trust is well-governed through its policies and procedures ensuring they are up to date and fit for purpose.
Management consult and negotiate with staff representatives on appropriate Trust policies and procedures and propose and formulate policies and procedures in partnership. All policies are appropriately reviewed, updated, and maintained, following legislative changes and good employment practice. An equality impact assessment is also mandatory for all policies.
The effectiveness and performance of all policies are reported through the relevant sub committees of the Board for oversight and assurance.
Disabled persons
The Workforce Disability Equality Standard covers measures that enable the Trust to compare the experiences of disabled and non-disabled staff. This informs an action plan to support positive change and a more inclusive environment for disabled staff.
The action plan for 2024 to 2025 was reported and monitored by the Diversity and Inclusion Steering and Advisory Group (DISAG) on a quarterly basis. The action plan is published on the Trust’s public-facing website.
The Workforce Race Equality Standard (WRES) was introduced in 2015 and is a set of specific measures (metrics) that enables NHS organisations to show progress ensuring employees from black and minority backgrounds have equal access to career opportunities and receive fair treatment in the workplace.
The WRES continues to prompt enquiry and assist the Trust to develop and implement evidence-based responses to the challenges revealed by its data.
Following data analysis, a WRES action plan was developed covering the period April 2024 to March 2025 and progress on that is monitored quarterly.
The WRES metrics and associated action plan is published on the Trust’s public-facing website.
The Trust is committed on meeting and is delivering on the statutory and mandated requirements under the Equality Act 2010 and accompanying standards as required by NHS England and Improvement.
Control measures are in place to ensure that all the organisation’s obligations under equality, diversity and human rights legislation are complied with.
Staff turnover
Latest data published by NHS England shows that WMAS continues to set the benchmark for staff retention, proudly achieving the lowest leaver rate among all ambulance trusts in the country. This achievement reinforces our commitment to making WMAS a great place to work by promoting staff wellbeing, investing in personal development, and fostering a culture of compassion and inclusivity.
Retaining experienced staff ensures that patients receive expert care, in the right place at the right time. Staff retention is more than just a metric, it’s the foundation of continuity, experience, and quality in patient care which can only be achieved by listening to staff and taking action to improve their employee experience.
WMAS turnover at the end of March 2025 for the rolling 12 month period was 6.84%.
Trade Union Facility Time 2023 to 2024
The Trade Union (Facility Time Publication Requirements) Regulations 2017 requires NHS Foundation Trusts to report annually a range of data in relation to their usage and spend on trade union facility time.
The facility time data for West Midlands Ambulance Service University NHS Foundation Trust, for the period 1 April 2023 to 31 March 2024, the latest data available, is shown below.
Total number of employees who were TU representatives
73 64.73 Full-Time Equivalent
Percentage of time spent on facility time
0% 29 employees
1%-50% 39 employees
51%-99% 3 employees
100% 2 employees
Percentage of pay bill spent on facility time
Total cost of Facility Time £198,764
Total pay bill £310,016,000
Percentage of the total pay bill
spent on facility time, calculated as:
(total cost of facility time ÷ total pay bill)
x 100 0.06%
Time spent on paid TU activities as a percentage of total paid facility time hours
35.46% calculated as total hours spent on paid TU activities by TU representatives during the relevant period ÷ total paid facility time hours) x 100.
The figures have been calculated using the standard methodologies used in the Trade Union (Facility Time Publication Requirements) Regulations 2017.
Expenditure on consultancy
£126k was spent on consultancy during 2024 to 2025, compared to £202k in 2023 to 2024.
Off payroll arrangements
An ‘Off Payroll’ arrangement is where contracted individuals are paid directly or through their own companies and so are responsible for their own tax and NIC arrangements. They are not classed as employees.
It is the Trust’s policy that all off-payroll engagements are subjected to a risk based assessment as to whether assurance is required that the individual is paying the correct amount of tax and, where necessary, that the assurance has been sought.
Prior to commencement, for each engagement the individual must have signed a contract stating that they are responsible for accounting for the relevant taxes, national insurance, liabilities, charges and duties.
Notwithstanding this, the Trust would not agree to such arrangements except in very exceptional circumstances, and there were no such arrangements in 2024 to 2025 (2023 to 2024 none).
Table 1: Highly paid off-payroll worker engagements as of 31 March 2025 earning £245 per day or greater
| No. of existing engagements as of 31 March 2025, of which … | Nil |
| No. that have existed for less than one year at time of reporting. | Nil |
| No. that have existed for between one and two years at time of reporting. | Nil |
| No. that have existed for between two and three years at time of reporting. | Nil |
| No. that have existed for between three and four years at time of reporting. | Nil |
| No. that have existed for four or more years at time of reporting. | Nil |
Table 2: All highly paid off-payroll workers engaged at any point during the
year ended 31 March 2025 earning £245 per day or greater
| Number of off-payroll workers engaged during the year ended 31 March 2025, of which | Nil |
| Not subject to off-payroll legislation* | Nil |
| Subject to off-payroll legislation and determined as in-scope of IR35* | Nil |
| Subject to off-payroll legislation and determined as out of- scope of IR35* | Nil |
| Number of engagements reassessed for compliance or assurance purposes during the year, of which | Nil |
| number of engagements that saw a change to IR35 status following review | Nil |
*A worker that provides their services through their own limited company or another type of intermediary to the client will be subject to off-payroll legislation and the Trust must undertake an assessment to determine whether that worker is in-scope of Intermediaries legislation (IR35) or out-of-scope for tax purposes.
Table 3: For any off-payroll engagements of board members, and/or senior officials with significant financial responsibility, between 1 April 2024 and 31 March 2025
| Number of off-payroll engagements of board members, and/or senior officials with significant financial responsibility, during the financial year. | Nil |
| Number of individuals that have been deemed ‘board members and/or senior officials with significant financial responsibility’ during the financial year. This figure must include both off-payroll and on-payroll engagements. | 7 |
Staff Exit Packages (subject to audit)
Reporting of compensation schemes – exit packages 2024 to 2025
| Exit package cost band (including any special payment element) | Number of compulsory redundancies | Number of other departures agreed | Total number of exit packages |
|---|---|---|---|
| <£10,000 | 0 | 0 | 0 |
| £10,000 – £25,000 | 0 | 1 | 1 |
| £25,001 – 50,000 | 0 | 1 | 1 |
| £50,001 – £100,000 | 0 | 0 | 0 |
| £100,001 – £150,000 | 0 | 0 | 0 |
| £150,001 – £200,000 | 0 | 0 | 0 |
| >£200,000 | 0 | 0 | 0 |
| Total number of exit packages by type | 0 | 2 | 2 |
| Total cost (£) | £0 | £53,000 | £53,000 |
Reporting of compensation schemes – exit packages 2023 to 2024
| Exit package cost band (including any special payment element) | Number of compulsory redundancies | Number of other departures agreed | Total number of exit packages |
|---|---|---|---|
| <£10,000 | 0 | 0 | 0 |
| £10,000 – £25,000 | 0 | 2 | 2 |
| £25,001 – 50,000 | 0 | 0 | 0 |
| £50,001 – £100,000 | 0 | 0 | 0 |
| £100,001 – £150,000 | 1 | 0 | 1 |
| £150,001 – £200,000 | 0 | 0 | 0 |
| >£200,000 | 0 | 0 | 0 |
| Total number of exit packages by type | 1 | 2 | 3 |
| Total cost (£) | £127,000 | £21,000 | £148,000 |
Exit packages: other (non-compulsory) departure payments 2024 to 2025
| Exit packages: other (non-compulsory) departure payments | Payments Agreed £000 | Total value of agreements £000 |
|---|---|---|
| 0 | 0 | |
| Voluntary redundancies including early retirement contractual costs | 0 | 0 |
| Mutually agreed resignations (MARS) contractual costs | 0 | 0 |
| Early retirements in the efficiency of the service contractual costs | 0 | 0 |
| Contractual payments in lieu of notice | 0 | 0 |
| Exit payments following Employment Tribunals or court orders | 0 | 0 |
| Non-contractual payments requiring HMT approval | 2 | 53 |
| Total | 2 | 53 |
| Of which: Non-contractual payments requiring HMT approval made to individuals where the payment value was more than 12 months’ of their annual salary | 0 | 0 |
Exit packages: other (non-compulsory) departure payments 2023 to 2024
| Exit packages: other (non-compulsory) departure payments | Payments Agreed £000 | Total value of agreements £000 |
|---|---|---|
| 0 | 0 | |
| Voluntary redundancies including early retirement contractual costs | 0 | 0 |
| Mutually agreed resignations (MARS) contractual costs | 0 | 0 |
| Early retirements in the efficiency of the service contractual costs | 0 | 0 |
| Contractual payments in lieu of notice | 0 | 0 |
| Exit payments following Employment Tribunals or court orders | 0 | 0 |
| Non-contractual payments requiring HMT approval | 2 | 21 |
| Total | 2 | 21 |
| Of which: Non-contractual payments requiring HMT approval made to individuals where the payment value was more than 12 months’ of their annual salary | 0 | 0 |
Gender Pay Gap
All organisations with more than 250 employees are required to report annually on their gender pay gap. The gender pay gap shows the difference in average pay between all men and women in the workforce
The gender pay gap is different to equal pay which deals with the pay differences between men and women who carry out the same jobs. A particularly high gender pay gap can indicate issues that need to be addressed, and the individual calculations may help to identify what those issues are.
The Trust’s approach to pay supports fair treatment and reward of all staff irrespective of gender.
A full Gender Pay Gap Report is published on the Trust’s public-facing website.
Staff Survey
NHS staff survey background
The NHS staff survey is conducted annually. From 2021 to 2022 the survey questions align to the seven elements of the NHS ‘People Promise’, retaining two previous themes of engagement and morale. All indicators are based on a score out of 10 for specific questions with the indicator score being the average of those.
Approach to staff engagement
The 2024 NHS Staff Survey fieldwork was open for 11 weeks at WMAS, from 16th September to 29th November 2024. It was administered by Picker Europe Ltd and was conducted as a census.
For the last eight years WMAS ran the survey electronically for ease of access to all staff. A unique link to the survey questionnaire is sent by email to each individual staff. The completed questionnaire is then submitted securely and anonymously to the contractor for processing.
6922 staff were invited to take part in the 2024 staff survey and 4697 staff returned a completed survey compared to 2261 in 2023.
A number of actions were taken before and during the survey to encourage staff to take part and share their views, these included: –
- Announcements through the Weekly Briefing prior to the survey launch.
- Weekly “You Said, Together We Did” posters about how survey results are used
- People Promise Drop-In sessions at different localities
- Pull-up banners at different Trust events to raise awareness
- Weekly results from Picker Europe were shared widely to show progress
- Posters and video information were shared by managers with their teams
- Weekly emails were sent to managers to remind them to keep encourage staff to
- Positive stories from staff about the survey shared in Weekly Briefing newsletter
- A live Questions and Answers session was organised on MS Teams
Staff survey response rates
This year 2024 to 2025 68%
Last year 2023 to 2024 40%
Notable statistics on response rates
- The response rate increased from 40% in 2023 to 2024 to 68% in 2024/25
- Significant increase in the number of BAME staff responses (24/25 357 v147 23/24)
- The average response rate for all Ambulance Trusts is 49% compared to 52% in 2023 to 2024
Staff survey results
| Indicators People Promise | Trust Score 2024 to 2025 | Bench-mark group score 2024 to 2025 | Trust Score 2023 to 2024 | Bench-mark group score 2023 to 2024 | Trust Score 2022 to 2023 | Bench-mark group score 2022 to 2023 |
|---|---|---|---|---|---|---|
| We are compassionate and inclusive | 6.61 | 6.84 | 6.55 | 6.90 | 6.38 | 6.71 |
| We are recognised and rewarded | 5.20 | 5.25 | 5.09 | 5.38 | 4.79 | 5.05 |
| We each have a voice that counts | 5.93 | 5.98 | 5.88 | 5.98 | 5.75 | 5.85 |
| We are safe and healthy | 5.70 | 5.65 | 5.57 | 5.61 | 5.37 | 5.37 |
| We are always learning | 4.79 | 4.98 | 4.86 | 4.86 | 4.63 | 4.56 |
| We work flexibly | 5.18 | 5.45 | 5.14 | 5.30 | 4.72 | 5.03 |
| We are a team | 5.97 | 6.25 | 5.94 | 6.21 | 5.70 | 6.05 |
| Staff engagement | 5.80 | 6.01 | 5.78 | 6.02 | 5.61 | 5.90 |
| Morale | 5.77 | 5.63 | 5.57 | 5.56 | 5.36 | 5.23 |
Local results of the 2024 Staff Survey
- A total of 119 questions were asked in the 2024 survey, of these, 113 can be compared to 2023 and 101 can be positively scored.
- Responses to 10 questions are better than last year, and responses to 15 questions are worse than 2023.
- Overall, there is no significant improvement in the positive responses compared to last year’s results.
- Compared to other Ambulance Trusts that used Picker as their survey contractor, WMAS scored significantly worse in 62 questions.
| Top 5 scores | WMAS 2024 | WMAS 2023 |
|---|---|---|
| q3h. I have adequate materials, supplies, and equipment to do my work | 70% | 67% |
| q10c. I don’t work any additional unpaid hours per week for this organisation, over and above contracted hours | 73% | 67% |
| q23a. I received an appraisal in the past 12 months | 90% | 92% |
| q3i. There are enough staff at organisation to do my job properly | 44% | 35% |
| q24f. I am able to access clinical supervision opportunities | 54% | N/A |
| Most Improved Scores | WMAS 2024 | WMAS 2023 |
|---|---|---|
| q3i. There are enough staff at organisation to do my job properly | 44% | 35% |
| q14b. I have not experienced harassment, bullying or abuse from managers | 88% | 82% |
| q10c. I don’t work any additional unpaid hours per week for this organisation, over and above contracted hours | 73% | 67% |
| q14a. I have not experienced harassment, bullying or abuse from patients/service users, their relatives, or members of the public | 51% | 46% |
| q14c. I have not experienced harassment, bullying or abuse from other colleagues | 83% | 79% |
| Bottom 5 scores | WMAS 2024 | WMAS 2023 |
|---|---|---|
| q11e. I have not felt pressure from manager to come to work when not feeling well enough | 53% | 54% |
| q9d.My immediate manager takes a positive interest in my health and well-being | 50% | 53% |
| q9e. My immediate manager values my work | 48% | N/A |
| q9b. My immediate manager gives clear feedback on my work | 45% | 46% |
| q6d. I can approach my immediate manager to talk openly about flexible working | 50% | 50% |
| Most declined scores | WMAS 2024 | WMAS 2023 |
|---|---|---|
| q9e. My immediate manager values my work | 48% | 53% |
| q10b. I don’t work any additional paid hours per week for this organisation, over and above contracted hours | 23% | 27% |
| q24a. My organisation offers me challenging work | 58% | 62% |
| q24b. There are opportunities for me to develop my career in this organisation | 45% | 49% |
| q13a. I have not experienced physical violence from patients/service users, their relatives, or other members of the public | 61% | 65% |
Commentary on key findings
The key findings that were seen as a priority by the People Voice Action Group and the Task and finish group led to the creation of the Trust Action Plan with three key priorities. The scores for leadership and management decreased significantly since 2023. The bullying and harassment results improved significantly since 2023; however it was felt that we still needed to keep working on this area and also sexual safety to continue to build on the great work that is already in place. There are still some concerns with physical violence which is being addressed from a different perspective compared to last year.
Future priorities, targets and action plans
Priorities are decided locally with relevant staff in each locality through Listening into Action groups and staff meetings. The People Voice Action Group (PVAG) meets regularly to interrogate the results and make recommendations for organisation-wide actions.
Three key priorities have been agreed by the SSRAG and the Executive Membership Board to focus on following the 2023 Staff Survey Results.
Safe Environment Action Plan
Key Deliverables are: –
- A healthier and safer environment will be created for staff to thrive and perform their duties to their best potential and deliver the best patient care
- Create a safe environment for staff to thrive and ensure our leaders lead with compassion and civility.
- Staff will feel they are being listened to by their leaders and have reassurance that our leaders are committed to ensure the safety of staff at work.
- Staff will be aware of the support available to them and be assured that the Trust will prosecute those who demonstrate physical violence towards our staff.
- Improvement in the confidence level seen in the staff survey, through our peope feeling more confident to speak up because all processes are enacted in the right way.
Leadership and Management Action Plan
Key Deliverables are: –
- Leaders will be better equipped to lead with compassion and civility and understand how behaviours may be perceived differently than intended. Staff will feel more supported by line managers which will increase staff engagement.
- Leaders will be more visible and approachable to staff and will be seen to demonstrate the behaviours that we want other staff to adopt.
- Female leaders will be more visible and approachable to staff.
- Staff will be more aware of senior leaders within the organisation and how their roles fit within the wider organisational structure.
- Increased capacity to support staff wellbeing and hold important conversations. Staff will feel valued and supported.
- Staff will be well informed of actions that are taken in response to their feedback. Staff will have an increased sense of engagement, involvement, advocacy and be more likely to make suggestions to improve their area of work.
Staff Welfare Action Plan
Key Deliverables are: –
- A healthier and more engaged workforce feeling supported to deliver the best patient care.
- Staff will feel more trusted and supported with their health and wellbeing.
For the full results of the WMAS Staff Survey please see below links :-
Results | Working to improve NHS staff experiences | NHS Staff Survey
Local results for every organisation | NHS Staff Survey
Freedom to Speak Up
West Midlands Ambulance University NHS Foundation Trust (The Trust) is committed to ensuring that staff have the confidence to raise concerns and to know that they will be taken seriously and investigated. At work, it is reasonable that staff may have concerns from time to time, which normally can be resolved easily and informally. However, when staff have serious concerns about unlawful conduct, financial/professional malpractice, or risk to patients/others it can be daunting to speak up about this. Therefore, the Freedom to Speak Up Policy aims to give staff the assurance that concerns will be listened to. This is supported by a simple procedure which demonstrates a fair and easy process for staff to raise concerns at work.
To deliver high quality patient care and protect the interests of patients, staff and the organisation, the Trust aims to encourage a culture of openness and transparency, in which members of staff feel comfortable about raising legitimate concerns. It is hoped that by providing clear procedures and channels for staff to raise concerns, issues can be addressed at the earliest opportunity, in the most appropriate way, so that positive steps can be taken to resolve them and reduce future risk.
FTSU Guardians
The Trust employs a Lead Guardian and a Guardian who are responsible for implementation of FTSU arrangements, liaising with staff, students, volunteers and managers throughout the organisation. Pippa Wall and Lucy Butler are registered with the National Guardian’s Office and are members of the West Midlands Guardian Network, and the National Ambulance Network (NAN), ensuring that good practice is followed and shared.
FTSU Ambassadors
There are currently approximately 63 trained ambassadors around the region, an increase from 50 in the previous year. We have at least one Ambassador per site who are known and trusted members of both the FTSU team and local teams. This helps to ensure that staff feel more comfortable discussing their concerns informally. The Ambassadors play a key role in the provision of our service across the geography that we serve. They attend regular developmental sessions and are encouraged to provide their own expertise in service developments. Digital posters showing the local Ambassadors’ photographs and personal statements are displayed on all sites.
Governance
There are number of ways in which assurance is provided for FTSU:
- Quarterly returns to National FTSU Guardian’s Office
- Regular discussions with the Chief Executive Officer, Chairman and the Executive and Non-Executive Leads for FTSU
- Quarterly reports to WMAS Learning Review Group and Quality Governance Committee, and bi-annual reports to the People Committee, Executive Management Board and Board of Directors
- NHS England’s Reflection and Planning Tool, presented to Board of Directors in May and October 2023, and confirmed as complete by Board of Directors in January 2024.
- National Guardian’s Office training modules are in place as follows:
- All staff completed Speak Up as part of Mandatory Training during 2023 to 2024
- Staff on Bands 7 – 8B are required to complete Listen Up Module
- Staff on Bands 8C and above, and Board of Directors have completed Listen Up and Follow Up modules
- Ambassadors are required to complete Speak Up and Listen Up training modules, in addition to their induction training
Concerns Raised 2024 to 2025
2024 to 2025 saw the highest number of concerns in a single year with a total of 131 concerns raised. This compares to 82 in the previous year. We believe the continuing increase in concerns relates, in part, to our regular promotional activities and team briefings to both staff and managers.
These were from the following service areas:
- Emergency and Urgent 39 (increase from 26 in 2023 to 2024)
- Patient Transport Services 16 (decrease from 17 in 2023 to 2024)
- Integrated Emergency and Urgent Care 33 (increase from 20 in 2023 to 2024)
- Other Departments 10 (increase from 9 in 2023 to 2024)
- Not stated 33 (increase from 9 in 2023 to 2024)
Among these concerns, the following were recorded (some concerns were recorded in multiple categories). The categories shaded grey are benchmarked nationally by the National Guardian’s Office.
| Reporting Category | E&U | IEUC | PTS | Other | Not stated | Grand Total | % of Total (2024 to 2025) |
|---|---|---|---|---|---|---|---|
| Patient Safety / Quality (Including clinical safety, health and safety) | 9 | 6 | 2 | 2 | 5 | 24 | 18.3% |
| Bullying / harassment | 6 | 2 | 3 | 0 | 9 | 20 | 15.3% |
| Worker Safety (including Health and Wellbeing, Psychological Safety, health and safety) | 26 | 15 | 8 | 6 | 15 | 70 | 53.4% |
| Other Inappropriate Attitudes or Behaviour | 19 | 14 | 6 | 4 | 12 | 55 | 42.0% |
| Detriment | 2 | 0 | 1 | 0 | 0 | 3 | 2.3% |
| Cultural | 5 | 2 | 1 | 1 | 7 | 16 | 12.2% |
| Sexual Safety | 2 | 0 | 2 | 0 | 3 | 7 | 5.3% |
| Diversity and Inclusion | 7 | 3 | 3 | 1 | 6 | 20 | 15.3% |
| Enquiry and advice | 1 | 0 | 1 | 2 | 0 | 4 | 3.1% |
| Fraud | 3 | 0 | 0 | 0 | 2 | 5 | 3.8% |
| Training | 3 | 1 | 0 | 0 | 3 | 7 | 5.3% |
| Behaviour of Peers | 12 | 11 | 5 | 1 | 14 | 43 | 32.8% |
| Behaviour of Management | 16 | 22 | 1 | 4 | 11 | 54 | 41.2% |
| Positive Improvement Suggestions | 3 | 0 | 1 | 2 | 0 | 6 | 4.6% |
| Other | 2 | 1 | 1 | 0 | 3 | 7 | 5.3% |
| Systems / processes (including HR, procedural) | 21 | 14 | 9 | 6 | 9 | 59 | 45.0% |
The most reported category is Worker Safety. Concerns recorded within this group include matters such as health and wellbeing, psychological safety, health and safety. This is followed by those relating to inappropriate attitude and / behaviour of either managers or colleagues.
Freedom To Speak Up remains one of many routes available to staff, students and volunteers to raise concerns, start conversations or provide positive suggestions or praise. During the last year, we have worked with other teams within the Trust to implement a guide to raising concerns, providing staff with examples of types of concerns and the routes that would be appropriate to each example.
A data breach incident has been reported, which occurred in November 2024, relating to Ambassador conversations. No individual cases which had been brought to the FTSU Guardians were breached. A small amount of personal data was inaccurately made available to the Trust’s trained FTSU Ambassadors, on a restricted access site. This was identified and reported by an ambassador, and access to the data was immediately removed. An incident report was completed, and a full review was carried out jointly with the IT Department. Actions to prevent such a breach from re-occurring were planned and implemented.
Corporate Governance
Code of governance
The Code of governance for NHS provider trusts (‘Code of governance’) sets out a common overarching framework for the corporate governance of NHS providers (being NHS trusts and NHS foundation trusts), reflecting developments in UK corporate governance and the development of integrated care systems. Providers must comply with each of the provisions of the code or, where appropriate, explain in each case why the provider has departed from the code.
The purpose of the Code of Governance is to assist in improving governance practices by bringing together the best practice of public and private sector corporate governance. The code is issued as best practice advice but imposes some disclosure requirements.
The Trust has applied the principles of the NHS Code of Governance on a ‘comply or explain’ basis. The NHS Code of Governance most recently published in April 2023, is based on the principles of the UK Corporate Governance Code.
The Directors of the Trust are responsible for preparing the Annual Report and Accounts. The Board of Directors consider that the Annual Report and Accounts, taken as a whole, is fair, balanced and understandable and provides the information necessary for patients, regulators, and stakeholders to assess West Midlands Ambulance Service University NHS Foundation Trust’s performance, business model and strategy.
Each individual who is a director are required to make themselves aware of any relevant audit information and to establish that the Trust’s Auditor is aware of that information, and as far as each individual Director is aware, there is no relevant audit information of which the Trust’s Auditor is unaware. ‘Relevant audit information’ means information needed by the Trust’s Auditor in connection with preparing their report.
A statement of the accounting policies for pensions and other retirement benefits are set out in a note to the accounts and the details of senior employees’ remuneration can be found in the Remuneration Report above.
The Trust has not made any use of financial instruments during the period of this Annual Report.
Governance, Leadership and Regulation
The Governance framework of a Foundation Trust is set out in Schedule 7 to the NHS Act 2006 as amended. It sets out an obligation to have:
- A Membership
- A Council of Governors
- A Board of Directors
- Specific directors on the Board
- Committees required under regulation
There are two main regulators that hold NHS Foundation Trusts to account for the quality of care they deliver and how they are run:
The Care Quality Commission (CQC) is the independent regulator of health and social care services.
NHS England (NHSE) through its NHS provider licence, regulates providers of NHS services.
The Trust is a licenced provider and is compliant with the conditions of the licence.
The Licensee now has a legal duty to co-operate with other providers of NHS services; and other NHS bodies, including any Integrated Care Board of which it is a partner.
The National Health Service Act 2006 (the Act) designates the Chief Executive of an NHS Foundation Trust as the Accounting Officer. The Accounting Officer is responsible for: –
- Keeping proper accounting records
- preparing the compliant financial statements
- Ensuring the trust delivers efficient and economical conduct of its business
- Safeguards financial propriety and regularity throughout the organisation
- Ensuring financial considerations are fully taken into account in decisions taken by the foundation trust.
- Acting as the principal advisor to the Board on these matters.
The Membership
The membership is the means by which the Foundation Trust is accountable to its local community. The Trust maintains a database of members and this database is cleansed regularly. The constituencies of the membership are set out in the Constitution of the Foundation Trust.
The Trust has circa 15,935 members; this includes both public members and staff members. WMAS operates an opt-out membership for its staff. This means that staff who are eligible for membership are automatically members of the Foundation Trust unless they choose to opt out.
| CONSTITUENCY | PUBLIC MEMBERS |
|---|---|
| Birmingham | 2,049 |
| Black Country | 2,791 |
| Staffordshire | 1,353 |
| West Mercia | 1,575 |
| Coventry and Warwickshire | 1,077 |
| Category | Membership as at 28/02/25 |
|---|---|
| Staff | 7,056 |
| Public | 8,879 |
| Total | 15,935 |
The Trust has a duty to involve the local community in decisions that affect them. This includes planning, developing and managing services as well as activities that aim to improve health or reduce health inequalities.
Members are requested to complete a membership form with the information providing information including on the Protected Characteristics under the Equalities Act 2010.
Further details on Patient and Public involvement are included within the Trust’s Quality Account which is published separately.
The Trust also produces a Members’ Newsletter to engage with members. Members of the Foundation Trust and members of the public may contact Governors via the Membership and Governor Engagement Manager [email protected].
The Council of Governors
As an NHS Foundation Trust, West Midlands Ambulance Services has a Council of Governors (CoG). This is a body of both elected and appointed members representing the interests of trust members (public and staff) and local organisations, holding non-executive directors accountable and approving significant decisions.
Governor elections last took place during the autumn of 2023 and the term of office of all elected and appointed Governors is three years from 1st January 2024.
The Chair of the Board of Directors is also Chair of the Council of Governors.
The Council of Governors is the accountable forum between the Board of Directors and the Trust’s Membership and key stakeholders. It represents local interests as well as staff and key partnership stakeholders.
The most significant obligations and duties of Governors are: –
- Hold the Non-Executive Directors individually and collectively to account for the performance of the Board Directors.
- Represent the interests of the members of the Trust as a whole and the interests of the public.
- Appoint or remove the Chair and the other Non-Executive Directors.
- Determine the remuneration and allowances, and the other terms and conditions of office, of the Non-Executive Directors.
- Appoint or remove the External Auditor.
Board Engagement with the Council of Governors (CoG)
- The Board of Directors recognises the importance of receiving and responding to the views of the Council of Governors. As a Foundation Trust, the Board of Directors is keen to understand the statutory powers of the Council of Governors and to support it in creating the forums where the Council can hold the Non-Executive Directors to account for the performance of the Trust. The Board of Directors’ papers are available to all members of the Council of Governors.
- Non-Executive Directors have attended meetings of the Council of Governors, and in addition the Trust has established a Governor/Non-Executive Director Buddy scheme. The publicly elected Governors are buddied with a respective Non-Executive Director. Meetings should take place facilitated by the Non-Executive Director with any views or comments flowing back through the meetings of the Non-Executive Directors for action or, if urgent, through the relevant Director into the Trust. Feedback will be through the same route.
- An update from the Chair and Chief Executive Officer is a standing item on the Council of Governors’ agenda where the Chair can report back on salient matters affecting the Board, the Trust and the Council of Governors.
Key Council of Governors (CoG) matters during 2024 to 2025
The Council of Governors is required to meet at least four times a year to discharge its duties and during 2024 to 2025 four were held meetings. Governor attendance is shown below.
In the period covered by this Annual Report, the Council of Governors discharged many of its statutory duties, including re-appointment and review of Non-Executive Directors remuneration.
At is meeting on 31st July 2024, Eileen Cox was elected unopposed as Lead Governor, and Khalid Ali was elected unopposed as Deputy Lead Governor for the period of one year until the next Annual Meeting.
Over the year, the Council of Governors received presentations from Trust Directors providing information to ensure that the Council fully understands the business of the Trust. The Chairman and Chief Executive Officer personally present to the Governors at every meeting.
Papers for Council of Governors meetings are available on the Trust’s website.
Attendance at meetings of the Council of Governors from April 2024 to March 2025 is presented below. The elected term of all the Governors listed is 1 January 2024 to 31 December 2026.
| Name | Constituency/Job Title | Attendance out of 4 meetings |
|---|---|---|
| Peter Brookes | Publicly Elected Governor – Birmingham | 2 |
| Khalid Ali | Publicly Elected Governor – Birmingham | 4 |
| Dave Murray | Publicly Elected Governor – Black Country | 3 |
| Anthony Bradley | Publicly Elected Governor – Black Country | 4 |
| Brian Murray | Publicly Elected Governor – Coventry and Warwickshire | 3 |
| John Davies | Publicly Elected Governor – Coventry and Warwickshire | 4 |
| Brenda Richards | Publicly Elected Governor – West Mercia | 3 |
| Roy Aldcroft | Publicly Elected Governor – West Mercia | 1 |
| Eileen Cox | Publicly Elected Governor – Staffordshire | 4 |
| Robin Cooke | Publicly Elected Governor – Staffordshire | 3 |
| Sarah Lawson | Staff Elected Governor – Emergency and Urgent Operational Staff | 4 |
| John Auerbach | Staff Elected Governor – Emergency and Urgent Operational Staff | 4 |
| Inderpal Sindhu | Staff Elected Governor – Non-Emergency Operational Staff | 3 |
| Duncan Spencer | Staff Elected Governor – Emergency Operations Centre Staff | 4 |
| Matt Brown | Staff Elected Governor – Support Staff | 3 |
| David Fitton | Appointed Governor – Community First Responder Regional Forum | 3 |
| Cllr Ed Lawrence | Appointed Governor – Local Authority | 3 |
The Board of Directors
The Board of Directors is responsible for formulating and driving strategy, ensuring accountability and shaping culture. It is ultimately accountable for everything that goes on in the organisation. Key activities of the Board also include risk management, establishing organisational culture and values, and financial reporting and controls.
As a licensed provider, the Board of Directors, as part of the NHS system must have regard to the triple aim of the NHS. The triple aim refers to the aim of achieving:
- Improve health and wellbeing for people, including addressing health inequalities
- Improve the experience and quality of care for individuals and families
- Use NHS resources sustainably and improve value for the system
The Board is the key place where all the aspects of governance (clinical, financial, workforce, staffing, information, research etc.) come together.
Policies governing who has authority to make decisions
The key governing documents of the organisation are its standing financial instructions, which ensure financial transactions are conducted legally and efficiently, and the scheme of delegation, which ensure clarity on where authority lies to make decisions.
The schedule of matters reserved for the Board of Directors sets out the matters delegated to the Chief Executive and those retained by Board and also matters that are referred to the Council of Governors.
Composition of the Board
The appointments required by regulation to the Trust’s Board of Directors are:
- A Non-Executive Director Chair
- A Chief Executive (and Accounting Officer)
- A Director of Nursing
- A Medical Director who must be a registered medical practitioner.
- A Finance Director
Good practice guidance advises appointing: –
- A Non-Executive Director with clinical experience to provide appropriate challenge on quality.
- At least one member of the Audit Committee to have recent and relevant financial experience.
The Trust is compliant with the above requirements and good practice.
Duties and Codes of Conduct
All Foundation Trusts have the following individual statutory duties:
- a general duty to promote the success of the Trust; and
- the duties to avoid conflict of interests, not to accept any benefits from third parties and to declare interests in any transactions that involve the FT.
The following codes of conduct and duties are upheld by Trust Directors’
- Code of Conduct based on the Nolan Principles
- Fit and Proper Persons test
- The Duty of Candour
All Directors on the Board of Directors and all Governors on the Council of Governors meet the “Fit and Proper” Person’s test described in the provider licence, and in relation to directors all meet the requirements of the CQC fundamental standards guidance. Both Directors and Governors are subject to a “Disclosure and Barring Service” check.
Declarations of Interest
The Board and the Council of Governors have adopted the “Managing Conflicts of Interest in the NHS: Guidance for staff and organisations” published by NHS England.
Upon appointment, members of the Board of Directors are asked to declare any business interests, directorships, positions of authority in a charity or voluntary body in the field of health and any connection with contracting bodies for NHS services.
They are also asked to declare their independence as defined by NHSE’s Code of Governance.
All declarations of interest are entered in a register which is updated at least twice a year and published on the Trust’s website.
Trust Board Skills Audit
Each year, Board members undertake a skills audit to ensure that that the Board remains fit for purpose and to provide appropriate guidance in terms of succession planning. A risk based succession plan is in place.
The Skills Audit Matrix assesses the membership of the Board of Directors against a number of key themes and skill areas that are agreed by the Board of Directors to be required for the stewardship of the Foundation Trust.
The audit provides assurance that the Trust complies with the NHS Leadership Competency Framework for Board members.
Each Executive Director and Non-Executive Director hold the following skills:
- Strategic Leadership
- Informed and Sound Judgment
- Ethics, Integrity and Accountability
- Impact and Influence
- Risk Management
- Financial acumen
- Knowledge and Application of Diversity and Inclusion
Below are specific skills / experience of each Board member. The last skills audit of the Board was undertaken in March 2025.
Non-Executive Directors
| Skill | Professor Ian Cumming | Mohammed Fessal | Mushtaq Khan | Julie Jasper | Narinder Kooneruntil 4th November 2024 | Professor Alexandra Hopkins | Suzanne Banksfrom 1st April 2024 | Sukhjeeven Natfrom 5th November 2024 |
|---|---|---|---|---|---|---|---|---|
| Financial qualification | no | no | no | yes | no | no | no | yes |
| Public policy | yes | yes | yes | yes | yes | yes | yes | no |
| Knowledge and Application of Diversity and Inclusion | yes | yes | yes | yes | yes | yes | yes | yes |
| Clinical and Health Experience | yes | yes | no | no | no | yes | yes | no |
| Health Experience: non Clinical | no | no | yes | yes | no | no | no | no |
| Legal awareness | no | yes | yes | yes | no | no | no | no |
| Corporate Communications and Media | no | no | yes | yes | yes | no | no | no |
| Commercial focus | no | no | yes | yes | yes | no | no | yes |
| Human Resource Management | yes | no | no | no | yes | no | no | no |
| Clinical Registration/ Professional Membership | Chartered Scientist – The Science CouncilFellowship of the Institute of Biomedical SciencesHCPC Registered – Biomedical Scientist, PIN: BS31759 | General Pharmaceu-tical Council – PharmacistPIN: 2061184 | The Law Society [England and Wales] SRA ID:26073 | Chartered Institute of Public Finance and Account-ancy | None | Master of Science in the Faculty of Medicine Nursing & Midwifery Council registrationPIN 0573742 | Nursing & Midwifery Council registration PIN 83C0111E | None |
| Professional/ BusinessQualification/ Experience | MSc in Sports and Exercise MedicinePgDip in Sports and Exercise MedicineDoctor of Health (DH)Doctor of Science (DSc)Doctor of the University (D Univ)CSci – Charter Scientist Qualification | Master of Sciences of PharmacyIndependent Prescriber Course | Solicitor (England & Wales); BSc. (Hons) Social Policy; Post Graduate Diploma in Law; Legal Practice Certificate, Post graduate Diploma in Management Studies; Certificate in Advanced Corporate Governance. | Qualified Accountant | Business Experience. Local Authority Councillor | Master of Business Administra-tion in Higher Education Management Doctor of Philosophy | Quality Service Improvement and Redesign Practitioner Post Grad Certificates in Strategic Workplace Planning and Higher & Professional EducationBSc in HealthcareMBA in Health Executive | BA Honours in Accounting and Information SystemsRBS Advanced Diploma Financial Planning Certificates |
Executive Directors
| Skill | Anthony Marsh | Karen Rutter (Voting) | Dr Alison Walker Medial Director(Voting)until 30 Nov 2024 | Carla Beechey(Voting) | Nathan Hudson(Voting) |
|---|---|---|---|---|---|
| Financial qualification | no | yes | no | no | no |
| Public policy | yes | no | no | no | no |
| Diversity and Inclusion | no | no | no | yes | no |
| Clinical and Health Experience | yes | no | yes | no | yes |
| Health Experience: Non Clinical | no | yes | no | yes | no |
| Legal awareness | no | yes | no | yes | no |
| Corporate Communications and Media | yes | no | no | no | no |
| Commercial focus | yes | no | no | no | no |
| Human Resource Management | yes | no | no | yes | no |
| Clinical Registration/ Professional Membership | None | Chartered Institute of Management Accounts | GMC Registration 4210643 | Chartered Institute of Personnel Development (MCIPD) | HCPC Registered Paramedic (PIN PA00832) |
| Professional/ Business Qualification/ Experience | National Ambulance Strategic Advisor Extended Ambulance Aid [NHSTA] (former Paramedic)MSc Strategic Leadership, MBA. MA.Honorary Professor of Emergency Services Management | Qualified accountant (CIMA) with associated designation of Chartered Global Management Accountant | Emergency Medicine (A&E) Consultant. MB BChir, FRCEM, FIMCRCS, FRCS, FDSRCS, MA, MFSEM. Dip Health Research, Cert Medicolegal. | Post Graduate DiplomaHuman Resource Management | MBA Executive Leadership Post Graduate Diploma Health and Social Care ManagementMulti Agency Gold Incident Command |
| Skill | Vivek Khashu | Murray MacGregor | Nick Henry | Caron Eyre (Voting) | Dr Richard Steyn (Voting)from 1st Dec 2024 |
|---|---|---|---|---|---|
| Financial qualification | no | no | no | no | no |
| Public policy | yes | no | no | no | no |
| Diversity and Inclusion | yes | no | no | yes | yes |
| Clinical and Health Experience | no | no | yes | yes | yes |
| Health Experience: Non Clinical | yes | yes | no | no | no |
| Legal awareness | no | no | no | no | no |
| Corporate Communications and Media | yes | yes | no | no | no |
| Commercial focus | yes | no | no | no | no |
| Human Resource Management | yes | no | no | yes | no |
| Clinical Registration/ Professional Membership | None | None | HCPC Registered Paramedic (PIN PA02768) | Registered Nurse (Adult) NMC PIN 86D0621E | GMC Registration 2921688 |
| Professional/ Business Qualification/ Experience | BSc Medical Biochemistry MSc Healthcare Leadership | None | MSc Healthcare Management (current study)Professional Development DiplomaMulti Agency Gold Incident Command | Msc in Clinical PracticePost Grad certificate in Workforce PlanningBSc in Nursing Studies | Consultant Thoracic Surgery/Major Trauma ServiceMBChB, MS, FRCSEd(C-Th) FIMCRCSEd, MRCGP, DRCOG |
Performance Evaluation of the Board and Directors
Development for directors appointed to the Board commences at induction, the content of which is reviewed by the Chairman and the Chief Executive Officer. The Board of Directors reviews its performance as a Board at the end of each meeting.
As a Foundation Trust, it is the role of the Council of Governors to ensure that there is an effective and meaningful performance assessment and appraisal process in place for both the Chair and Non-Executive Directors.
The Trust Chairman appraises the performance of the Chief Executive Officer annually and also carries out a mid-year review against objectives set by the Remuneration and Nominations Committee. The Chairman has also carried out an appraisal of each of the Non-Executive Directors. The Senior Independent Director undertook the appraisal of the Chairman.
The Chief Executive Officer appraises the performance of each Executive Director annually and also carries out a mid-year review against previously agreed objectives.
Executive and Non-Executive Director responsibilities
The Board comprises Non-Executive and Executive Directors whose principal responsibilities are summarised below.
Trust Board Member Responsibilities:
| Non-Executive Directors | Executive Directors |
|---|---|
| Nominated NED for Security Management. Emergency Officer NED required under the NHS England Emergency Preparedness, Resilience and Response Framework.Senior Independent Director.Safeguarding Lead.Learning from Deaths Lead.Freedom to Speak Up Lead. NED Lead Director to support the executive lead director for maternity services. Complaints and FTSU Auditor.NHS Workforce Well Being Guardian.Lead NED for Diversity and Inclusion.Sustainability Lead. Security Management NED Champion (including safety and risk) (see NHSE guidance Dec. 2021, covers: Counter Fraud, violence and aggression, security management of assets and estate). | Accounting Officer.Accountable Officer for Emergency Preparedness.Director of Infection Prevention and ControlCaldicott GuardianBoard Level Champion for maternity services. (Better Births Report).Senior Information Risk Owner (SIRO).Prevent and Safeguarding Executive Lead.Director for Health, Safety and Risk.Security Management Director (SMD).Controlled Drugs Accountable OfficerResponsible Officer (this is part of medical revalidation).Responsible Director CQC.Registration Authority (Smart Cards).Equality, Diversity & Human Rights.Patient Group Directives (PGDs).Freedom to Speak Up. Executive Nurse.Sustainability.Learning from Deaths Responsible Executive.Learning Disabilities and Mental Health.NHS Workforce Well Being Guardian. |
Current leads for SIRO, Caldicott Guardian and FTSU:
Senior Information Responsible Officer (SIRO)
The must be an Executive Director or Senior Management Board Member, this duty has been carried out by Karen Rutter (Director of Finance).
Caldicott Guardian
Responsible for protecting the confidentiality of patient or service-user information and enabling appropriate information sharing. They usually have a clinical background. The Medical Director undertakes this role for the Trust.
Freedom to Speak Up (FTSU) leads and Guardians
Suzanne Banks is the nominated Non-Executive Director and Vivek Khashu is the nominated Executive Director for Freedom to Speak Up during the period of this Annual Report. Pippa Wall and Lucy Butler are the Freedom to Speak Up Guardians.
Non-Executive Directors
Non-Executive Directors (NEDs) contribute to the development of strategy and play an important role in scrutinising the management in achieving agreed goals and objectives and monitoring the reporting of performance.
Drawn from the local community and living or working within the area covered by the Trust, NEDs also have a role in working with the Chair in the appointment and remuneration of the Chief Executive and other Executive Directors as members of the Trust’s Remuneration and Nominations Committee.
NEDs are considered independent by the Trust based on the NHSE Code of Governance.
All Non-Executive Director appointments to the Board of Directors are made by the Council of Governors for a period of three years as required by the Constitution.
- Professor Ian Cumming – period of office expires on 31 March 2027
- Alexandra Hopkins – period of office expires on 31 March 2026
- Narinder Kooner – retired from Board 4 November 2024
- Sukhjeeven Nat (replaced Narinder Kooner) – period of office expires on 4 November 2027
- Mushtaq Khan – period of office expires on 30 September 2025
- Mohammed Fessal – period of office expires on 31 December 2026
- Julie Jasper – period of office expires on 12 October 2025
- Suzanne Banks – period of office expires on 31 March 2027
The Chair held meetings with the Non-Executive Directors without the Executive Directors present, although the CEO takes the opportunity to provide a brief update on national and regional issues so that the NEDs are briefed on current matters.
At least one meeting a year is chaired by the Senior Independent Director without the Chair present as part of leading the annual appraisal of the Chair.
The Council of Governors agreed to link the NED remuneration to the Executive Directors “cost of living increase”.
Profiles of Non-Executive Directors
Professor Ian Cumming OBE – Chair
Ian started his career in the NHS as a Healthcare Scientist Since then Ian has held a variety of NHS general management posts including three years as the Chief Executive of the NHS in the West Midlands. From 2012 to 2020, Ian was Chief Executive of Health Education England (HEE), the largest education and training organisation in the world, Ian has a personal interest in pre-hospital care and in sports medicine, an area in which he holds an MSc.
Suzanne Banks CBE – Non-Executive Director
Suzanne joined the Trust on 1 April 2024. She retired as Chief Nurse at Sherwood Forest Hospitals NHS Foundation Trust in 2019 following a successful career of 38 years. She worked as a General Nurse, Children’s Nurse and Health Visitor and gained her MBA at Keele University. She currently works at a national level in the NHS Supporting menopause care in the workplace.
Professor Alexandra Hopkins – Non-Executive Director
A nurse for 48 years, Alex qualified in 1980 and worked in cancer nursing as a staff nurse and ward sister until the early 1990s. Further study of nursing at Manchester University led her to qualify as a nurse teacher and she moved into nursing and health education full time. She was recently appointed as a visiting Professor in Nursing and Health at Birmingham Newman University. Alex has retained a passion for, and commitment to, promoting excellence in quality patient care.
Mushtaq Khan – Non-Executive Director
Mushtaq is a highly regarded solicitor who has served as the President of the Birmingham Law Society and holds extensive experience as a Board Director. With over two decades of legal practice, including leadership roles in both private and public sectors, he has earned accolades as a top lawyer in renowned legal directories like Chambers and Partners UK and the Legal 500 UK.
Mohammed Fessal – Non-Executive Director
Mohammed has been a NED at WMAS since 2021, during which time he has been the Chair of the People Committee. As a qualified pharmacist, Mohammed has over 18 years’ experience across the NHS, private and voluntary sectors. Currently Director of Pharmacy at CGL, a voluntary sector organisation specialising in substance misuse, homelessness, domestic violence and young people’s services, Mohammed is passionate about supporting the most vulnerable in society by empowering and tackling discrimination.
Narinder Kaur Kooner OBE NLP Prac. – Non-Executive Director (to 4 November 2024)
Narinder Kaur Kooner has been a local authority Councillor since 2006 and has held the prominent position of Assistant Leader of Birmingham City Council. Narinder is a Local Government Association Labour Peer and has previously been on the Executive of Sikh Assembly UK.
Julie Jasper – Non-Executive Director
Julie joined the Board of WMAS in October 2022 as a Non-Executive Director and Chair of the Audit Committee. She qualified as an Accountant in 1985 and has enjoyed a successful career in Senior and Executive Director roles in the Public, Private, Voluntary and Nationalised Industry sectors.
Sukhjeeven (Sukh) Nat – Non-Executive Director (from 5 Nov 2024)
Sukh is currently an Executive Director with Cynergy Bank joining them two years ago to aid the growth of the Commercial and Property Finance division. He has 20 years’ banking experience in commercial and residential real estate finance with the likes of Santander, NatWest and RBS group. Following an advertisement and interview process the Council of Governors appointed Sukh who took his seat on the Board of Directors on 5 November 2024.
Chief Executive Officer and Executive Directors
The Chief Executive through the Executive Directors has the day-to-day responsibility for managing the Trust and ensuring the Board’s decisions are implemented. The Board is then responsible for the oversight of performance of the Trust in terms of outcomes.
The National Health Service Act 2006 (the Act) designates the Chief Executive of an NHS Foundation Trust as the Accounting Officer. The Accounting Officer is responsible for: –
- Keeping proper accounting records
- preparing the compliant financial statements
- Ensuring the trust delivers efficient and economical conduct of its business
- Safeguards financial propriety and regularity throughout the organisation
- Ensuring financial considerations are fully taken into account in decisions taken by the foundation trust.
- Acting as the principal advisor to the Board on these matters.
Executive Directors share the same corporate responsibilities as Non-Executive Director colleagues but bring detailed knowledge of the organisation’s management systems and processes and of the health sector, as well as specialised clinical and managerial expertise.
Anthony Marsh – Chief Executive
Anthony Marsh started his Ambulance Service career in Essex in 1987. Anthony has held several senior posts with the Ambulance Service in Hampshire, Lancashire, Greater Manchester and West Midlands. Anthony holds three master’s Degrees: an MSc in Strategic Leadership, a master’s in business administration (MBA) and a Master of Arts. Anthony also holds the National Portfolio for Emergency Planning, Response and Resilience and is the lead for the National Ambulance Resilience Unit.
Karen Rutter – Director of Finance
Karen is a qualified accountant with over 30 years’ experience in NHS finance. Karen is also the Trust’s Senior Information Risk Owner (SIRO) and Proud Network Executive Sponsor. Karen is a member of the Chartered Institute of Management Accounts (CIMA) with associated designation of Chartered Global Management Accountant.
Caron Eyre – Director of Nursing
Caron has more than 30 years of experience in nursing and is a Registered NMC Nurse. She has spent her entire career in the West Midlands starting in Birmingham, moving to Warwick and Worcestershire and then back to Birmingham. She is an adult and children’s nurse and a nurse tutor.
Dr Richard Steyn – Interim Medical Director (to 30 November 2024) and Medical Director (from 1 December 2024)
Richard has worked within the NHS since 1984. He initially trained and worked as a rural General Practitioner on the West of Scotland before subsequently moving into surgical training and was appointed as a Consultant Thoracic Surgeon at Birmingham Heartlands Hospital in 1999. Following a competitive recruitment selection process, Richard took up the position of substantive Medical Director on 1 December 2024
Dr Alison Walker – Medical Director (to 30 November 2024)
Alison has worked in the NHS for over 30 years. She is a Consultant in Emergency Medicine with a Specialist interest in Prehospital Care. She was a regional NHS Ambulance Service Medical Director from 2005 to 2013 and has worked with WMAS from 2010 both as an Interim Medical Director and Honorary Medical Advisor, later becoming Executive Medical Director in 2019. Alison announced her intention to retire from the Board of Directors and stepped down with effect from 30 Nov. 2024.
Nathan Hudson – Director of Performance and Improvement
Nathan Hudson is one of the Trust’s strategic commanders and has worked for West Midlands Ambulance Service since 1992. He started his career as part of the non-emergency patient transport service before moving to the emergency side of the Trust and qualified as a paramedic in 1997. Nathan is also a Multi-Agency Gold Incident Commander.
Carla Beechey – Director of People
Carla has over 20 years’ experience of working in the Human Resources profession having previously worked in the Further Education Sector. She joined WMAS in 2008 as an HR Advisor after completing her professional qualifications in Human Resources Management at the University of Wolverhampton.
Directors – Non-Voting Members
Vivek Khashu – Strategy and Engagement Director
Vivek started his career straight from university on the NHS Graduate Management Training scheme. Vivek has held a number of operational management posts in Acute Hospitals around the country and has also worked at a national level with NHS England and Improvement.
Murray MacGregor – Communications Director
Murray MacGregor has been working in the media and public relations since 1995, with the last 18 years as Communications Director for WMAS. During that time, he has overseen a significant upgrade in the way the Trust’s internal communications are handled and has helped raise the profile of the organisation within the Region and nationally.
Nick Henry – Paramedic Practice and Patient Safety Director
Nick started his career in 1990 with WMAS at the age of 16 years on their Cadet scheme in Birmingham whilst gaining experience in every department of the service including first contact with patients. He went on to qualify as a paramedic in 1995. Nick has worked in almost every area of frontline operations across the whole region. Nick joining the Trust Board in early 2023 as a Director is the pinnacle of a 32 year career. Nick has a wealth of Clinical and Health experience and is a Registered Paramedic and is studying for a MSc in Healthcare Management.
The Trust under its Constitution is required to put in place an indemnity for Directors and Governors to cover the risk of legal action against its directors, governors and appropriate officers. This insurance cover is in place.
Board Assurance
This section of the report describes the key governance and assurance mechanisms the Trust relies upon
A key job of the Board is to seek assurance that risks to its strategic objectives are known and that there are clear plans in place to mitigate, eliminate or manage those risks. This is done through submission of its Board Assurance Framework which is reviewed regularly.
Governance is the system by which the Trust is directed and controlled. The Board of Directors is responsible for overseeing the governance of the Trust. This includes setting the Trust’s Strategic Objectives and providing the leadership to put those Objectives into effect.
The Governance Framework enables the Board of Directors to supervise the management of the Trust. It is to be distinguished from the day-to-day operational management of the Trust by full-time executives.
Governance is primarily conducted and orchestrated through the leadership and functions of the Board. It is however the business and concern of everyone in the organisation.
The Annual Governance Statement sets out the means by which the Trust manages risk and how it is entrenched in the governance of the Trust. The Annual Governance Statement sets out clear responsibilities for quality of patient care.
Board Assurance Framework
The Board Assurance Framework (BAF) is the key source of evidence that links the Trust’s “mission critical” strategic objectives to risks, controls and assurances. It is the main tool that the Board uses in discharging its overall responsibility for internal control.
The BAF sets out the significant risks identified by the Trust, current mitigating actions and internal and external assurances. It also identifies control systems and processes and further mitigating actions to be taken for each risk area.
Whilst quantitative data assurance is essential, the Board also uses of soft or qualitative data that involves more personal interaction to source as a means of gaining assurance e.g., both Executive and Non-Executive Directors are invited to undertake several site visits in the year based on the principles of “Ward to Board”
Board meetings include a regular patient and staff experience story item on the ordinary meeting agenda to highlight matters that have gone well and those that have not gone so well. This is considered a key element of organisation learning
Sub-Committees of the Trust Board of Directors
- Audit Committee
- Finance and Performance Committee
- Quality Governance Committee
- Executive Management Board
- Remuneration and Nominations Committee
- People Committee
- Trustee Committee
- Council of Governors.
The Board gains its assurance through its committee structure. Committees : –
- Are chaired by non-executive directors that report directly to the Board
- Provide forums for detailed scrutiny of clinical, operational, and financial performance
- Provide assurance of compliance with Foundation Trust registration requirements
- Alert the Board to any significant risks and assurance on maintaining compliance
- Structures are reviewed annually
- Terms of Reference are available upon request from the Trust Secretary
The Trust has six sub committees, these are: –
| Committee | Responsibilities |
|---|---|
| Audit committee* | Ensuring the integrity of financial reporting, risk management, and internal controls. |
| Finance and performance committee | Oversight and scrutiny of performance of the Trust on matters of financial and operational performance. |
| Quality Governance Committee | Ensuring that appropriate standards are set and compliance with them is monitored on a timely basis. |
| Remuneration and Nominations Committee* | Agree on behalf of the Board individual remuneration, allowances and terms of service arrangements for the Chief Executive and Executive Directors. |
| People Committee | Provide assurance on the quality and impact of people, workforce and organisational development strategies and the effectiveness of people management. |
| Trustee Committee | Ensuring funds within the Trust’s registered charity are managed in accordance with relevant legislation and regulations. |
*Committees which are required under the constitution.
During 2024 to 2025, the Board of Director’s reviewed the Committee structure, its support network and Terms of Reference. The outcome of the review will be reported to the Board.
External Audit
Bishop Fleming (External Auditors since 1 November 2023) comply with the National Audit Office’s Code of Audit Practice. The Trust does not commission non-audit services from its external auditor
Integrated Care System
WMAS is hosted by the Black Country Integrated Care Board (ICB), however WMAS is a key stakeholder across all six of the ICS areas we serve, with the Black Country ICB leading as the host, this is to simplify working relationships when working at the scale of a region. The Black Country ICB hosts the regional commissioning team for the West Midlands when it comes to the commissioning of 111 and 999 services as part of this arrangement, it has done from the inception of ICBs and was hosted in its predecessor bodies too.
The Trust measures its performance at Trust and individual ICS level using an executive scorecard, it also shares this information with all six ICBs, NHS England and the Care Quality Commission on a monthly basis.
Directors are linked to ICSs and the Trust has a representative that is invited to attend the Trust’s lead ICB Board.
| ICS | Link Director | Title |
|---|---|---|
| Stoke and Staffs | Jeremy Brown | Emergency Operations Centre and Operational Planning Director |
| Coventry and Warks | Nick Henry | Paramedic Practice and Patient Safety Director |
| Black Country | Vivek Khashu | Strategy and Engagement Director |
| Birmingham and Solihull | Michelle Brotherton | Non-Emergency Patient Transport Services Operational Director |
| Shropshire | Caron Eyre | Director of Nursing |
| Hereford and Worcestershire | Vivek Khashu | Strategy and Engagement Director |
Whilst we have a host ICB and a lead commissioner, alongside the partnership arrangements across the ICBs, there are also professional networks, across finance, people, strategy and digital which take place, these all have senior representation from WMAS.
WMAS is a member on the Black Country ICB, with the Strategy and Engagement Director attending the ICB Board in a non-voting capacity.
In addition to the arrangements above, WMAS is also accountable to and regularly attends Health Overview and Scrutiny Committee meetings across the region, it is also an active participant in regional working groups chaired by NHS England, such as the regional Urgent and Emergency Care Board.
The formal oversight of WMAS is undertaken by our host ICB with participation of NHS England, this is undertaken through monthly System Review meetings and also Clinical Quality Review Group.
Board Meetings
Board Member Attendance at Meetings
The attendance at meetings during 2024 to 2025 of those who have served on the Board of Directors is as follows:
| Title of Meeting | Board of Directors | Executive Management Board | Audit Committee | Quality Governance Committee |
|---|---|---|---|---|
| Total Meetings | 6 | 25 | 6 | 5 |
NON-EXECUTIVE DIRECTORS
| Prof Ian Cumming (Chair) | 6/6 | Not applicable | Not applicable | Not applicable |
| Suzanne Banks | 6/6 | Not applicable | 3/3 | 5/5 |
| Mohammed Fessal | 5/6 | Not applicable | Not applicable | 5/5 |
| Prof Alexandra Hopkins | 5/6 | Not applicable | Not applicable | 4/5 |
| Julie Jasper | 6/6 | Not applicable | 6/6 | Not applicable |
| Mushtaq Khan | 6/6 | Not applicable | 4/6 | Not applicable |
| Narinder Kooner (to 4.11.24) | 3/3 | Not applicable | 3/4 | Not applicable |
| Sukhjeeven Nat (from 5.11.24) | 3/3 | Not applicable | 2/2 | Not applicable |
EXECUTIVE DIRECTORS
| Anthony Marsh | 6/6 | 19/25 | 1/1 | Not applicable |
| Carla Beechey | 6/6 | 23/25 | Not applicable | Not applicable |
| Caron Eyre | 4/6 | 14/25 | Not applicable | 3/5 |
| Nathan Hudson | 6/6 | 18/25 | Not applicable | Not applicable |
| Karen Rutter | 6/6 | 22/25 | 6/6 | Not applicable |
| Dr Richard Steyn (from 1.12.24) | 4/4 | 12/13 | Not applicable | 3/5 |
| Dr Alison Walker (to 30.11.24) | 3/3 | 9/12 | Not applicable | 2/3 |
NON-VOTING MEMBERS
| Nick Henry | 5/6 | 21/25 | Not applicable | 4/5 |
| Murray MacGregor | 5/6 | 20/25 | Not applicable | Not applicable |
| Vivek Khashu | 6/6 | 23/25 | Not applicable | 2/5 |
| Title of Meeting | People Committee | Finance and Performance Committee | Remuneration and Nominations Committee | Trustee Committee |
|---|---|---|---|---|
| Total Meetings | 4 | 5 | 3 | 3 |
NON-EXECUTIVE DIRECTORS
| Prof Ian Cumming (Chair) | Not applicable | Not applicable | 3/3 | Not applicable |
| Suzanne Banks | 4/4 | Not applicable | 3/3 | 3/3 |
| Mohammed Fessal | 3/4 | Not applicable | 3/3 | 3/3 |
| Prof Alexandra Hopkins | 4/4 | Not applicable | 2/3 | 3/3 |
| Julie Jasper | 1/1 | 4/5 | 3/3 | 2/3 |
| Mushtaq Khan | Not applicable | 5/5 | 3/3 | 3/3 |
| Narinder Kooner (to 4.11.24) | Not applicable | 3/3 | 2/2 | 2/2 |
| Sukhjeeven Nat (from 5.11.24) | 3/3 | 2/2 | 0/1 | 1/1 |
EXECUTIVE DIRECTORS
| Anthony Marsh | Not applicable | Not applicable | 3/3 | 3/3 |
| Carla Beechey | Not applicable | Not applicable | 3/3 | 3/3 |
| Caron Eyre | Not applicable | Not applicable | Not applicable | 2/3 |
| Nathan Hudson | 4/4 | 5/5 | Not applicable | 3/3 |
| Karen Rutter | Not applicable | 5/5 | Not applicable | 3/3 |
| Dr Richard Steyn (from 1.12.24) | 4/4 | Not applicable | Not applicable | 1/1 |
| Dr Alison Walker (to 30.11.24) | 3/3 | Not applicable | Not applicable | 2/2 |
NON-VOTING MEMBERS
| Nick Henry | 3/4 | Not applicable | Not applicable | Not applicable |
| Murray MacGregor | Not applicable | Not applicable | Not applicable | Not applicable |
| Vivek Khashu | Not applicable | Not applicable | Not applicable | Not applicable |
The Board meets formally, both in public and private sessions throughout the year to discharge its duties.
Papers for Board meetings are available on the Trust’s website.
Matters are considered by the Board in public and only by exception would an item be considered in private session. Items considered in private would include those matters not normally disclosed under a Freedom of Information request.
NHS Oversight Framework
As an NHS Foundation Trust, West Midlands Ambulance Service is subject to the regulatory framework established by NHS England, the independent regulator of NHS and NHS Foundation Trusts. That framework covers both financial and governance risks.
NHS England’s NHS Oversight Framework provides the framework for overseeing Integrated Care Boards and providers and identifying potential support needs. The framework looks at five themes
- Quality of care, access and outcomes.
- Preventing ill health and reducing inequalities.
- People.
- Finance and use of resources; and
- Leadership and capability.
The aim of that framework is to facilitate NHS England’s assessment of there being:-
- a significant risk to the financial sustainability of a provider of key NHS services which endangers the continuity of those services and/or
- poor governance as an NHS Foundation Trust.
In 2022 to 2023 the NHS Oversight Framework was updated to reflect the statutory establishment of ICBs in July 2022 and to reflect their role in oversight.
The approach to oversight is characterised by the following key principles:
- Working with and through ICBs, wherever possible, to tackle problems
- Greater emphasis on system performance and quality of care outcomes, alongside the contributions of individual healthcare providers and commissioners to system goals
- Matching accountability for results with improvement support, as appropriate
- Autonomy for ICBs and NHS providers as a default position
- Compassionate leadership behaviours that underpin all oversight interactions informed by Our Leadership Way
Segmentation
The general nature and level of support an organisation requires is reflected in its ‘segmentation’ rating. WMAS currently has a segmentation rating of 2.
- Segmentation 1: No Support Requirements
- Segmentation 2: As above unless specific mandated support required (See note below)
- Segmentation 3: Mandated Support
- Segmentation 4: Mandated Intensive Support.
Note re the Trust’s current rating
During 2021 to 2022 NHS England nationally re-assessed all providers against the Single Oversight Framework and placed WMAS within segmentation 2, this was in recognition of the pressures resulting from, and support required to, address the significant deterioration in ambulance handover delays and the resulting lengthening response times.
The Trust is working closely with our six integrated care systems and NHS England to jointly address these two key issues.
Care Quality Commission Rating
Trust CQC rating: Good
WMAS remains fully compliant with the registration requirements of the Care Quality Commission (CQC) who inspected the Trust during 2023 to 2024 and is rated as Good.
CQC inspection
WMAS was inspected in 2023, the inspection looked at our leadership via the Well Led domain and also our core services, which included our control rooms and our 999 front line service. The outcome of the inspection was a rating of “Good” overall, with several aspects of outstanding practice noted, including for example our Control Rooms being rated as “Outstanding”.
Whilst the Trust was disappointed to receive a lower rating than that awarded in 2019, the current set of ratings are still the highest in the ambulance sector, the ratings breakdown is as follows:
Ratings for the whole Trust (published February 2024)
| Safe | Effective | Caring | Responsive | Well-Led | Overall |
|---|---|---|---|---|---|
| Good | Good | Outstanding | Good | Good | Good |
Ratings for Specific Services
| Safe | Effective | Caring | Responsive | Well-Led | Overall | |
|---|---|---|---|---|---|---|
| Emergency Operations Centre | GoodFeb 2024 | OutstandingFeb 2024 | GoodFeb 2024 | GoodFeb 2024 | OutstandingFeb 2024 | OutstandingFeb 2024 |
Resilience | GoodJan 2017 | OutstandingJan 2017 | Not Rated | OutstandingJan 2017 | OutstandingJan 2017 | OutstandingJan 2017 |
| Patient Transport Services | GoodAug 2019 | GoodAug 2019 | GoodAug 2019 | GoodAug 2019 | GoodAug 2019 | GoodAug 2019 |
| Emergency and Urgent Care | GoodFeb 2024 | Requires ImprovementFeb 2024 | OutstandingFeb 2024 | GoodFeb 2024 | GoodFeb 2024 | GoodFeb 2024 |
The full report can be found here : West Midlands Ambulance Service University NHS Foundation Trust – Overview – Care Quality Commission
Trust’s CQC Action Plan
The Trust has reviewed all recommendations contained in CQC published report on the outcome of their review. This was the subject of an action plan and oversight by the Executive Management Board as part of learning and development for the Trust or the Board especially in relation to a “well led” organisation.
Worcestershire Health and Care system inspection
In keeping with the CQCs strategy on risk-based inspection of pathways and systems, in addition to individual Trusts, on the evening of Monday 21 November, the CQC commenced a three day on-site inspection of the Worcestershire Health and Care system. West Midlands Ambulance Service, as a provider to this was included within this inspection.
The CQC have picked up on areas of commendable practice and care we can be proud of, they have also highlighted very real issues with patient safety, experience, and staff morale. This report will explore some of that in more detail, as whilst the observations are all accurate, the executive team have expressed concern to the CQC on a limited number of the recommendations.
The final report has been published on the CQC website.
Accounting officer’s statement of responsibilities
The NHS Act 2006 states that the chief executive is the accounting officer of West Midlands Ambulance Service University NHS foundation trust. The relevant responsibilities of the accounting officer, including their responsibility for the propriety and regularity of public finances for which they are answerable, and for the keeping of proper accounts, are set out in the NHS Foundation Trust Accounting Officer Memorandum issued by NHS England.
NHS England has given Accounts Directions which require West Midlands Ambulance Service University NHS Foundation Trust to prepare for each financial year a statement of accounts in the form and on the basis required by those Directions.
The accounts are prepared on an accruals basis and must give a true and fair view of the state of affairs of West Midlands Ambulance Service University NHS Foundation Trust and of its income and expenditure, other items of comprehensive income and cash flows for the financial year.
In preparing the accounts and overseeing the use of public funds, the Accounting Officer is required to comply with the requirements of the Department of Health and Social Care Group Accounting Manual and in particular to:
- Observe the Accounts Direction issued by NHS England, including the relevant accounting and disclosure requirements, and apply suitable accounting policies on a consistent basis
- Make judgements and estimates on a reasonable basis
- State whether applicable accounting standards as set out in the NHS Foundation Trust Annual Reporting Manual (and the Department of Health and Social Care Group Accounting Manual) have been followed, and disclose and explain any material departures in the financial statements
- Ensure that the use of public funds complies with the relevant legislation, delegated authorities and guidance
- Confirm that the annual report and accounts, taken as a whole, is fair, balanced and understandable and provides the information necessary for patients, regulators and stakeholders to assess the NHS foundation trust’s performance, business model and strategy and
- Prepare the financial statements on a going concern basis and disclose any material uncertainties over going concern.
The accounting officer is responsible for keeping proper accounting records which disclose with reasonable accuracy at any time the financial position of the NHS foundation trust and to enable them to ensure that the accounts comply with requirements outlined in the above mentioned Act. The Accounting Officer is also responsible for safeguarding the assets of the NHS foundation trust and hence for taking reasonable steps for the prevention and detection of fraud and other irregularities.
As far as I am aware, there is no relevant audit information of which the foundation trust’s auditors are unaware, and I have taken all the steps that I ought to have taken to make myself aware of any relevant audit information and to establish that the entity’s auditors are aware of that information.
To the best of my knowledge and belief, I have properly discharged the responsibilities set out in the NHS Foundation Trust Accounting Officer Memorandum.
Signed
Position: Chief Executive, Date: 23 June 2025
Annual Governance Statement
Scope of Responsibility
As Accounting Officer, I have responsibility for maintaining a sound system of internal control that supports the achievement of the West Midlands Ambulance Service University NHS Foundation Trust’s (WMAS) policies, aims and objectives, whilst safeguarding the public funds and departmental assets for which I am personally responsible, in accordance with the responsibilities assigned to me. I am also responsible for ensuring that WMAS is administered prudently and economically and that resources are applied efficiently and effectively. I also acknowledge my responsibilities as set out in the NHS Foundation Trust Accounting Officer Memorandum.
The Purpose of the System of Internal Control
The system of internal control is designed to manage risk to a reasonable level rather than to eliminate all risk of failure to achieve policies, aims and objectives; it can therefore only provide reasonable and not absolute assurance of effectiveness. The system of internal control is based on an ongoing process designed to identify and prioritise the risks to the achievement of the policies, aims and objectives of West Midlands Ambulance Service University NHS Foundation Trust, to evaluate the likelihood of those risks being realised and the impact should they be realised, and to manage them efficiently, effectively and economically. The system of internal control has been in place in West Midlands Ambulance Service University NHS Foundation Trust for the year ended 31 March 2025 and up to the date of approval of the annual report and accounts.
Capacity to handle risk
An understanding of the risks that face the Trust is crucial to the delivery of emergency and non-emergency healthcare services moving forward.
Risk management is a key component of enhancing patient care and is a central part of the Trust’s strategic management.
The Trust has in place a Risk Management Strategy which support the Trust’s Strategic and Operational plans are as follows:
- To ensure safe and timely systems for identifying, reporting and managing risks
- To facilitate timely feedback and learning from reported risks, incidents and near misses
- Board level ownership and assurance that risks are fully reviewed and well managed
- Promote open and transparent culture of risk management throughout the Trust
Every organisation has to accept a degree of risk. The Board determines the balance between mitigation, toleration and acceptance of unmitigated risk i.e., Risk Appetite.
The Trust Risk Appetite Statement is continually reviewed. The statement sets out the Board’s strategic approach to risk-taking by defining its overall risk appetite, its boundaries, risk tolerance, acceptance and threats to its Strategic Objectives and supports delivery of the Trust’s Risk Management Strategy and Policy.
Effective management of risk relies on adequate controls being in place to provide assurance. This is achieved through the Board Assurance Framework (BAF) which provides a comprehensive evidence base of compliance against internal and external standards, targets and requirements.
Register of interests
The foundation trust has published on its website an up-to-date register of interests, including gifts and hospitality, for decision-making staff (as defined by the trust with reference to the guidance) within the past twelve months as required NHS27 by the Managing Conflicts of Interest in the guidance.
Quality Impact Assessment
The Trust has an approved Quality Impact Assessment Framework and Equality Impact Assessment. These ensure that transformational programmes designed to provide improved efficiencies do not adversely impact on the quality of the service to patients.
CQC Compliance
The foundation trust is fully compliant with the registration requirements of the Care Quality Commission.
NHS Pension Scheme
As an employer with staff entitled to membership of the NHS Pension Scheme, control measures are in place to ensure all employer obligations contained within the Scheme regulations are complied with. This includes ensuring that deductions from salary, employer’s contributions and payments into the Scheme are in accordance with the Scheme rules, and that member Pension Scheme records are accurately updated in accordance with the timescales detailed in the Regulations.
Equality, diversity and human rights
Control measures are in place to ensure that all the organisation’s obligations under
equality, diversity and human rights legislation are complied with.
Climate change and Green Plan
The foundation trust has undertaken risk assessments on the effects of climate change and severe weather and has developed a Green Plan following the guidance of the Greener NHS programme. The trust ensures that its obligations under the Climate Change Act and the Adaptation Reporting requirements are complied with.
Identifying and Reporting Risk
Risk management involves the following main steps:
- identifying the significant risks that would prevent achievement of objectives
- assigning ownership
- evaluating the significance of each risk
- identifying suitable responses to each risk
- ensuring the internal control system helps manage the risks
- regular review
The Trust’s Risk Register and incident reporting are available for staff to view at any stage electronically, to encourages a culture of openness and willingness to admit when errors have been made.
The Board is kept aware of actual and potential risks through a system of robust, formal, and devolved reporting structures. This system provides a strong focus on evaluating and managing risk.
The Risk and Control Framework
Management of Risk
The Trust’s Risk Management Strategy includes guidance on the responsibility for the management of risks with clear guidance on the authority for treatment of risks. All staff have an important role to play in identifying, assessing and managing risk.
A Health, Safety and Risk Framework sets out safe working processes and hierarchy of control needed to ensure overall compliance with the Health and Safety at Work Act 1974 and relevant Regulations in support of the Health and Safety Executive (HSE) guidance. It aims to empower all Managers to understand and conduct risk assessments by defining:
- How risks threaten the achievement of the Trust Strategic Objectives
- Risk appetite, tolerance, levels of residual risk and acceptance.
- The Risk Strategy and associated Policies and Procedures
- How risk is managed within the Trust regardless of grade (low, medium, high)
- Duty of Care and responsibility for every Staff member within the Trust relating to risk management.
- Allocation of responsibility
- Identification, monitor and review of risks.
The Trust’s Risk Register identifies risks at four levels from 1 very low to 4 high risk
Regulation
As a Foundation Trust, the organisation operates under a licence, the revised licence and conditions came into effect on 1 April 2023. The Board of Directors and the Council of Governors have been made aware the revised conditions. The existing control and reporting mechanisms described in this Annual Governance Statement are used to ensure that the Trust is compliant with the terms of its licence.
The Board each year reviews its Annual Skills Matrix to ensure it has sufficient capability at Board level to provide effective organisational leadership on the quality of care provided. The skills matrix is presented in the Governance Disclosures section of this Annual Report. All Directors on the Board meet the “fit and proper” persons test as described in the provider licence issued by the Regulator and also the CQC fundamental standards requirements as set out in regulations. The Directors are asked each year to notify the Trust if circumstances have changed.
As required by regulation the Trust has an Audit Committee consisting of Non-Executive Directors. The Chairman of the Trust is not a member of the Audit Committee and attends at least once a year, with the Chief Executive by invitation to present the Annual Governance Statement. The Audit Committee at the conclusion of each meeting meets with the internal and external auditors without the presence of Executive Directors or staff. In addition, the Local Counter Fraud Specialist presents a report to every meeting of the Audit Committee on measures to tackle Fraud, Bribery and Corruption and also the importance of reporting concerns as appropriate.
The Trust also has a Remuneration and Nominations Committee consisting of the Non-Executive Directors and when appropriate the Chief Executive Officer is also required to attend in line with Regulation.
In addition, the following committees are not required by regulation but are considered good practice for NHS Boards. A Quality Governance Committee, a Finance and Performance Committee and a People Committee have been established and meets regularly. Each Committee is chaired by a Non-Executive Director. The approved Minutes of all Board Committees are reported to the next appropriate Board meeting where they are received.
Each Committee also has an identified lead Executive Director. The responsibilities of the Board and its Directors are defined in the Trust’s Constitution, Standing Financial Instructions and Standing Orders.
The Audit Committee submits an Annual Report to the Board of Directors and the Council of Governors, and, in addition, the Trust’s External Auditor presented an independent report to the Council of Governors and the Membership at its Annual Meeting in July 2024.
Bishop Fleming is engaged as the Trust’s External Auditors and KPMG is the Trust’s Internal Audit provider. Assurance for the 24-25 financial year is provided under these arrangements.
The Board has a detailed schedule of business, which is reviewed at each ordinary meeting of the Board. The schedule defines when reports will be submitted, ensuring the Board can carry out its duty of oversight. Key performance reports covering corporate, clinical, quality, workforce, finance and operational performance indicators are received at each ordinary meeting of the Board and are made available on the Trust’s website as part of the Trust Information Pack.
The Trust has in place Directorate Portfolios, and these are reviewed in the wake of any changes at senior level. There is a clear organisational structure with staff and managers identified within each directorate, who are sufficient in number and appropriately qualified.
The Trust governance structure is based on financial control, operational performance monitoring and assurance in relation to clinical quality governance.
The Trust Information Pack submitted to each ordinary meeting of the Board enables timely and effective scrutiny and oversight by the Board of the Licensee’s operations. This document is published on the website. In addition, directors have access to up-to-date operational information, as well as receiving the details of any serious incidents reported.
The Trust is compliant with health care standards that are binding which is demonstrated by the Trust being rated as “Good”.
As part of gaining assurance the Board members are encouraged to visit staff, with each director allocated to a particular Trust site. In addition, through the ‘Day in the Life’ programme the Members of the Board and the Council of Governors can attend operational shifts and meet patients and operational staff.
The Quality Governance Committee receives regular reports from clinical and operational staff and through a number of documents such as the serious incident reports, learning from deaths, claims and inquests and Learning Review Group update are able to have oversight and challenge the Trust in relation to the quality of patient care. The Trust’s Medical Director, the Paramedic Practice and Patient Safety Director and the Executive Director of Nursing advise the Committee.
Roles and Responsibilities
The Board of Directors hold overall responsibility for the management of risks within the Trust, ensuring significant risks to the Trust’s ability to provide a quality service are identified and managed. The Board at each meeting receives a Trust Information Pack that contains Key Performance indicators.
Non-Executive Directors seek assurance in relation to the performance of the Executive Management Board in meeting agreed goals and objectives.
Chief Executive Officer is the Accounting Officer and is responsible for ensuring that a system is in place for reporting of all incidents.
Executive Directors hold responsibility for the identification and management of their risks and ensure they are documented, registered and updated in a timely fashion for the relevant forums to review. They are responsible for the risk management process within the Trust.
Governance Director and Trust Secretary was during the period of the report responsible for Corporate Governance for the Foundation Trust and compliance with the Foundation Trust Constitution.
Director of Nursing during the period of the report was responsible for monitoring and review of the Risk Management Strategy and associated policies, provision of expert advice into the incident reporting process, and maintaining appropriate quality and clinical governance.
Paramedic Practice and Patient Safety Director provides strategic leadership and clinical advice to the Board including patient safety, learning from deaths etc.
The Director of People is responsible for ensuring all staff receive an adequate level of training in accordance with the Trust’s Training Needs Analysis (TNA).
Pillar Committees and Subgroups of the Trust provide a process for escalation of assurance and risk through The Trust.
Executive Management Board provides a support and challenge function which includes review of business cases, agreement of actions required including escalation of major and high-risk transformational change to the Board of Directors.
Audit Committee monitors financial risks and reviews the Board Assurance Framework. It critically reviews and reports on the relevance and robustness of the Governance structures and assurance processes on which the Board places reliance.
Finance and Performance Committee has responsibility for monitoring and reviewing the adequacy and utilisation of resources to assure the Board on the risks relating to the efficient and effective delivery of strategic financial and operational plans.
Quality Governance Committee reviews and monitors actions for Patient Safety Clinical, Health and Safety, Equipment etc.
Health, Safety, Risk and Environment Group reviews Risk Registers escalating high risks to the Quality Governance Committee. The Group ensures risks are managed per policy.
People Committee has specific responsibility for the management of risk relating to the employment and development of staff and will review the Workforce element of the Trust’s risk register at least four times each year.
Learning Review Group has responsibility for identifying and monitoring trends in incident reports, ensuring identified risks are delegated for assessment and management, ensuring learning from incidents are shared appropriately with all stakeholders, and reporting identified trends and issues to the Health Safety Risk and Environmental Group.
Professional Standards Group (PSG) ensures that risks relating to the Clinical and Quality strategies are reviewed, thus ensuring high quality clinical care continues to be delivered across the organisation. PSG ensures the organisation remains Safe, Effective and Responsive and that opportunities to further improve are reviewed and actioned accordingly.
Operational Management Team manages service delivery risks. They ensure that the risk assessments from the Trust’s Risk Register are maintained by the relevant manager.
Public Stakeholder involvement
WMAS engagement with local communities emphasises building relationships, trust and confidence in the organisation.
The Trust has several staff networks, where information has been shared on local and national developments around equality and inclusion. The networks are kept up to date on consultations and engagement where appropriate and form part of the Diversity and Inclusion Steering and Advisory Group (DISAG) which meets quarterly.
The networks are Disability, Carers and Advocates (DCA) network, ONE (BAME) network, Proud network, Military network, Women’s network, Student Network
The Trust also engages with local authority Health Overview and Scrutiny Committees, and also local Healthwatch organisations across the West Midlands.
The Trust’s Stakeholder Engagement Strategy provides a strategic framework for engagement with its key stakeholders. During consultation on the draft annual Quality Account, engagement meetings are arranged for the West Midlands region for various stakeholders – for example the public, ICBs, and Health Overview and Scrutiny Committees (HOSC).
The Trust’s website provides ready access to information across all areas of Trust activity. The Trust also uses its newsletter for members to inform the public of new developments and items of interest. Work has commenced on the website to make more accessible than currently.
Review of Economy, Efficiency and Effectiveness of the Use of Resources
The Trust secures the economic, efficient and effective use of resources through a variety of means:
- A well-established policy framework (including Standing Financial Instructions).
- An organisational structure which ensures accountability and challenge through the committee structure.
- An established planning process.
- Effective corporate directorates responsible for workforce, revenue and capital planning and control.
- Detailed monthly financial reporting including progress on achievement of Cost Improvement Programmes and year-end forecasting.
- A financial Investment Group that reviews the merits and risks of investments
- A Business Case “post implementation” review is undertaken and reported to Board.
Day to day management of resources is delegated through the Executive Management Board (EMB). EMB takes lead responsibility for the annual planning cycle – formulating the plan, implementing the plan, monitoring delivery against the plan, taking action to bring variances back under control and reporting.
The Board of Director’s Schedule of Business includes comprehensive reviews of performance against clinical, operational, workforce, corporate and financial indicators through the Trust Information Pack at each meeting. Any emerging issues are identified and mitigating action implemented.
The Finance and Performance Committee, which is Chaired by a Non-Executive Director with other Non-Executive Directors also members, provides assurance to the Board of Directors as to the achievement of the Trust’s financial plan and priorities and, in addition, acts as the key forum for the scrutiny of the robustness and effectiveness of all cost efficiency opportunities. It interfaces with the other Board Committees and the Trust Executive Management Board.
In response to the work undertaken to review use of NHS resources by Lord Carter and his team, the Trust established an Efficiency and Transformation Group led by the Chief Executive and the Director of Finance, which has responsibility for identifying the actions required to find new ways of improving efficiency and productivity whilst ensuring high quality clinical care continues to be delivered across the organisation.
The Trust’s commitment to value for money is strengthened by the effective and focused use of its Internal Audit service. Following a review of the Internal Audit Provision, KPMG have been engaged to undertake the Internal Audit service. The Internal Auditors provide an independent and objective assurance to firstly EMB, then through the Audit Committee assurance statements to the Board that the Trust’s risk management, governance and internal control processes are operating effectively.
By virtue of its size West Midlands Ambulance Service is able to employ a range of skills to ensure that the Trust in general and the Audit Committee in particular secures assurance that resources are being appropriately utilised.
The Trust has a Local Counter Fraud Specialist (LCFS) supported as required by other qualified Local Counter Fraud Specialists. Any concerns can be directed to the team and any information is treated in the strictest confidence.
External Auditors, Internal Auditors and Counter Fraud report to each meeting of the Audit Committee and also meet the members of the Audit Committee without Management present.
The EMB reviews the Annual Internal Audit Plan and also reviews the Clinical Audits and then receives draft audit reports prior to submission to the Audit Committee to enable a management response to be prepared.
NHSE is responsible for overseeing foundation trusts and NHS trusts, as well as independent providers that provide NHS-funded care. It offers the support the providers need to give patients consistently safe, high quality, compassionate care within local health systems that are financially sustainable.
Workforce Strategies and Systems
The Trust has an established Workforce Planning Team, consisting of senior members of the Operational, Finance and Workforce directorates, who ensure robust scrutiny and development of the workforce plan. This is completed with due regard to Commissioners’ future intentions. In support of this work the Trust has developed Workforce and Organisational Development strategies that have been endorsed by the Board of Directors.
Information Governance
There is currently a piece of work ongoing within the Information Governance Team to review, amend and update procedures and processes. This is with a view to both strengthen existing workflows but to also introduce efficiencies across the Trust. This includes:
- Refresh information governance and data sharing principles so that each Team is aware of their duty and expectation.
- Review policies, procedures, notices to ensure they are accurate, fully support regulatory requirements and are clear
- Introduce reference documents, process flows and “guides” for teams
- Trend management and reporting, and updating the categorisation
- Learning from incidents to mitigate and reduce risk e.g. data breaches.
The Medical Director undertakes the role of Caldicott Guardian for the Trust. They are the senior person responsible for protecting the confidentiality of patient and service-user information and enabling appropriate information-sharing. The Director of Finance is the nominated Senior Information Risk Owner (SIRO) for the Trust. The Head of Governance is the Data Protection Officer.
The Trust has a Data Security and Protection Toolkit (DSPT). All organisations that have access to NHS patient data and systems should publish a DSPT self-assessment to provide assurance that they are practicing good data security, and that personal information is handled correctly. West Midlands Ambulance Service has met all mandatory requirements and will publish its DSPT assessment for 2024 to 2025 in line with the June 2025 deadline.
The Trust continues to work on the NHS Data Security and Protection Toolkit (DSPT) for 2024 to 2025. The Trust completed and published its baseline assessment as required by the 28 February 2025.
The process for assurance of the DSPT was previously reviewed by internal audit and assurance was provided to the Trust’s Audit Committee. The submission of the DSPT is 30 June 2025. The Trust will receive regular reports on the progress of DSPT through the Health Safety Risk and Environmental Group, Quality Governance Committee, Executive Management Board and Trust Board. The Trust’s Head of Governance, Safety and Security reports the DSPT through to the Director of Finance and is responsible for management of the DSPT.
Training is provided to all staff, as part of annual mandatory training, on good information governance practices. Ad hoc notifications of active threats are communicated to staff via email, Trust intranet and ambulance hub message screens.
Annual Quality Report
The Directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 (as amended) to prepare Quality Accounts for each financial year. NHSE (in exercise of the powers conferred on Monitor) has issued guidance to NHS foundation trust boards on the form and content of annual Quality Reports which incorporate the above legal requirements in the NHS Foundation Trust Annual Reporting Manual.
The following arrangements are in place within the Trust to assure the Board that the Quality Account presents a balanced view and that there are appropriate controls in place to ensure the accuracy of data:
Governance and Leadership
The Trust during the period of this Annual Report had a Medical Director, a Director of Nursing and a Paramedic Practice and Patient Safety Director to advise the Board of Directors on all matters relating to the preparation of the Trust’s Annual Quality Account. The Director of Nursing has designated responsibility for the development of the quality agenda.
People and Skills
All staff involved in collecting and reporting on quality metrics are suitably trained and experienced.
The Business Intelligence Unit and Clinical Audit teams
Ensure data quality checking takes place prior to any published data reports.
Clinical reporting is regularly audited both internally and externally by the Internal and External Auditors and audits also take place with individual clinicians.
Data Use and Reporting
Quality Reports, which outline the Trust’s performance against key quality objectives including benchmarking and comparative data and are the subject of discussion and challenge at Trust Governance meetings up to and including the Board of Directors, to inform the annual Quality Account.
Policies and Plans in ensuring quality of care provided
Policies and procedures are in place in relation to the capture and recording of patient data. Regular monitoring and scrutiny takes place throughout the governance structure with assurance and risks managed and escalated as previously described.
Systems and Processes
Systems and processes are in place for the audit and validation of performance data.
Review of effectiveness
As Accounting Officer, I have responsibility for reviewing the effectiveness of the system of internal control. My review of the effectiveness of the system of internal control is informed by the work of the internal auditors, clinical audit and the executive managers and clinical leads within the NHS foundation trust who have responsibility for the development and maintenance of the internal control framework. I have drawn on performance information available to me. My review is also informed by comments made by the external auditors in their management letter and other reports. I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the board, the audit committee [and risk/clinical governance/quality committee, if appropriate] and a plan to address weaknesses and ensure continuous improvement of the system is in place.
The Board of Directors has put in place and annually reviews the Trust committee structure to ensure clear governance arrangements are in place, which is supported by Trust documentation. The approved Board Committee minutes are submitted to the subsequent Board meeting. Each executive director reports to each meeting of the Board on matters relevant to their portfolio. Regular reports are also provided through the Trust Information Pack which includes the following areas – financial control, patient experience, patient safety, serious incidents, duty of candour, safeguarding, medicines management, claims and coroners, Infection Prevention and Control, Freedom of Information, policies and procedures and non-patient safety incidents. The Board also receives a bi-annual report from the Freedom to Speak Up Guardian on whistleblowing and concerns raised by staff and volunteers.
The Audit Committee reviews the Trust’s risk management and internal control systems. It monitors the Board Assurance Framework, Risk Register and Internal Control processes through its own activities and through receiving relevant reports from the External and Internal Auditors. Risks are monitored at Executive Management Board, Audit Committee, Performance Committee, People Committee and the Quality Governance Committee, with high risks reported to Board. The Committee regularly reviews Internal Audit plans and reports in order to form an opinion on the effectiveness of internal control systems and to recommend acceptance by the Accounting Officer. In 2023 to 2024 the Audit Committee approved an Internal Audit Plan that gave a balanced focus on financial, operational and clinical governance. That plan allocated internal audit resources between governance and risk issues, finance, performance and operations, information governance, quality and clinical, and human resource reviews.
The Quality Governance Committee has primary responsibility for monitoring and reviewing quality and clinical aspects of performance and development plans together with associated risks and controls, corporate governance and quality/clinical outcomes and for providing assurance on them to the Board. For these aspects, the Committee ensures that appropriate standards are set and compliance with them is monitored on a timely basis. The Committee also ensures that relevant Key Performance Indicators, strategic and operational milestones and timescales, are identified and monitored for achievement and effectiveness. WMAS recognises the importance of ongoing evaluation of the quality of care provided against key indicators. As a member of the National Ambulance Service Clinical Quality Group (which develops National Ambulance Quality Indicators and National Clinical Audits), the Trust actively partakes in both national and local audits to identify improvement opportunities. As a result, the Trust has a comprehensive Clinical Audit Programme which is monitored by the Clinical Audit and Research Group.
Internal Audit undertake a range of reviews of internal processes and controls and management have fully accepted their findings and have agreed action plans to address/strengthen controls where required. The Audit Committee has considered all Internal Audit reports and monitors progress against any outstanding management actions.
The Head of Internal Audit provides me with an opinion on the overall arrangements for gaining assurance through the Assurance Framework and on the controls reviewed as part of the Internal Audit work. The Assurance Framework and the performance reports provide me with evidence that the effectiveness of the controls in place to manage the risks to the organisation achieving its strategic objectives have been reviewed.
Head of Internal Audit Opinion
Significant assurance with minor improvement opportunities can be given on the overall adequacy and effectiveness of the organisation’s framework of governance, risk management and control.
Date: 23 June 2025
Conclusion
I can confirm that no significant internal control issues have been identified in the body of the Annual Governance Statement above.
Signed: | |
| Position: | Chief Executive Officer |
| Date: | 23 June 2025 |